Background: Social isolation (SI) is a largely silent and unrecognized social determinant of health that has negative health outcomes, including increased mortality, depression, hospital readmissions, and emergency room visits. In addition, a recent study revealed that SI and loneliness (L) are self-reported as often as food and housing insecurity. While hospitals readily work on food and housing insecurity for hospitalized patients, most facilities do little to address SI and L. Indeed, very little is known about SI and L in hospitalized patients, particularly those patients hospitalized in safety net hospitals, as most research into these topics has centered on older, insured adults who live in the community. Therefore, we conducted a point prevalence study of SI and L and a series of focused patient interviews with adult inpatients at our hospital.
Purpose: Our objectives are:1. Measure the prevalence of SI and L within the inpatient population, and2. Understand how to best reduce SI and L.
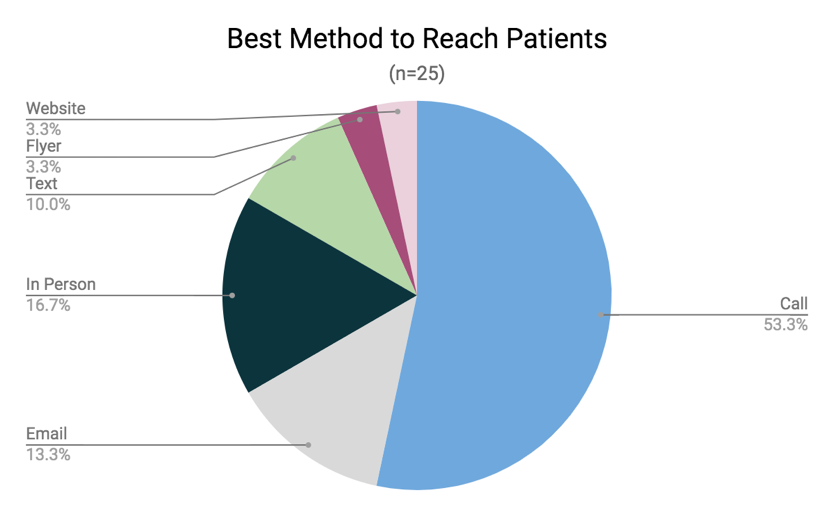
Description: We assessed the point prevalence of SI and L with a two-question screen of all willing and able adult patients (n=149) hospitalized in the LAC+USC Medical Center medical/surgical wards in the fall of 2019. As seen in Figure 1, 33 (22%) patients screened positive for SI only, 8 (5%) screened positive for loneliness only, and 30 (20%) screened positive for SI and L. For some patients we also conducted focused patient interviews that explored how to reduce SI and L. We assessed how to structure future interventions to reduce SI, including if patients would work with community navigators and the best method of communication after discharge. Of the 28 patients interviewed, 22 (79%) expressed interest in connecting with a community health worker/navigator or a local community-based resource center. The remaining patients were focused on more immediate concerns such as improved health or stable housing before pairing with a navigator. Since many of our patients have limited methods of communication due to lack of internet access, use of temporary cell phones, and frequent address changes, it is important to determine how to best connect patients to resources after they leave the hospital. As seen in Figure 2, the majority (53%) of our patients wanted to communicate by phone calls and in person support (17%). Email (13%) and text messaging (10%) were also preferred in our patients.
Conclusions: This project demonstrates the significant prevalence of SI and L within our hospitalized patients. It also highlights the need of our patients for an intervention that targets SI and L in a patient-centered manner, and communicates with them mainly through cellphone.