Background: Internal medicine and hospital medicine providers are under pressure to move patients quickly through the hospital and decrease length of stay. Providers spending most of their clinical time seeing patients, documenting or coordinating care and have minimal time to disrupt workflow to perform common bedside procedures such as paracentesis, lumbar punctures, central lines, arthrocentesis and thoracentesis. Combining this shift in clinical workflow with the ABIM’s stance on these procedures not being required to graduate residency, has led to providers being uncomfortable with performing these procedures.. Procedures then get redirected to subspecialty services or Interventional Radiology (IR) resulting in potential delays in patient care. We sought to tackle these problems with a pilot procedure service run by hospitalists at a large academic hospital with both teaching and direct care internal medicine service lines.
Purpose: Our mission was to start a dedicated procedure service to alleviate some of the issues. A cadre of well trained hospitalists can perform these procedures safely and efficiently. Through this endeavor we aim to improve throughput for hospitalized patients needing bedside procedures, standardize the performance of the procedure, provide direct observation and supervision to trainees, while providing a safe and efficient service to our patients. The downstream effects would lead to decreased length of stay, improved billing, decreased use of radiology suites for simple procedures.
Description: We started a 3-month pilot of a hospitalist run procedure service starting October 1, 2019. Five hospital medicine attending physicians were part of this pilot. The physicians underwent procedure training prior to the start of this pilot. The procedures offered were abdominal paracentesis, central venous catheter placement, lumbar punctures, arterial lines and arthrocentesis. Ultrasound equipment and physician time was funded through the Division of Hospital Medicine. Procedure service was available every day from 7am to 5pm, including weekends, through a dedicated pager. A survey was created to capture data for consult volume, completion, type of procedure and complications. Several other procedure specific and system specific data were collected. Data presented is at the halfway point for this ongoing pilot.
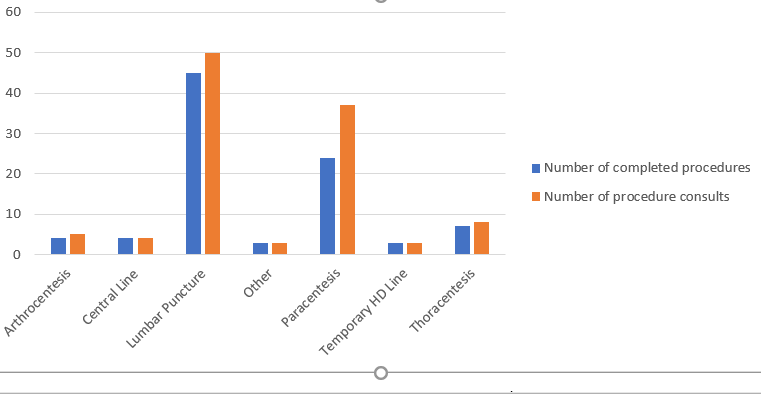
Conclusions: The procedure team was consulted 110 times in the first 44 days of this pilot. 90 procedures were completed. This comprised of 45(50%) lumbar punctures, 4 central venous lines, 4 arthrocentesis, 3 temporary hemodialysis access lines, 24(26%) abdominal paracentesis and 7 thoracentesis procedures. 44% of the procedures (41/90) involved supervising residents, the remainder were done directly by the procedure team.One week into the pilot, we started collecting data for “Anticipated delay if procedure team had not completed procedure”. 64 out of 81 (79%) completed procedures would have had anticipated delays of approximately 18hours per procedure. If the procedure team had not been an option, 36 out of 81 (44.4%) would have consulted Interventional Radiology, and 15 out of 81 (18.5%) would have consulted a subspecialty service. With this preliminary data, we expect to entirely deliver on our goals for this pilot. We are delivering safe and efficient bedside procedures, while assisting in throughput, assisting IR, supervising residents and avoiding service delays. We hope to present 3-month data, if accepted, at the annual meeting.