Background: Several electronic health record (EHR) mortality prediction models have been developed to promote early goals of care discussions (GOCD) but only a few models were evaluated prospectively. We aimed to implement a real-time 30-day inpatient mortality prediction model previously developed at our facility and evaluate its effect on GOCD in seriously ill transferred patients.
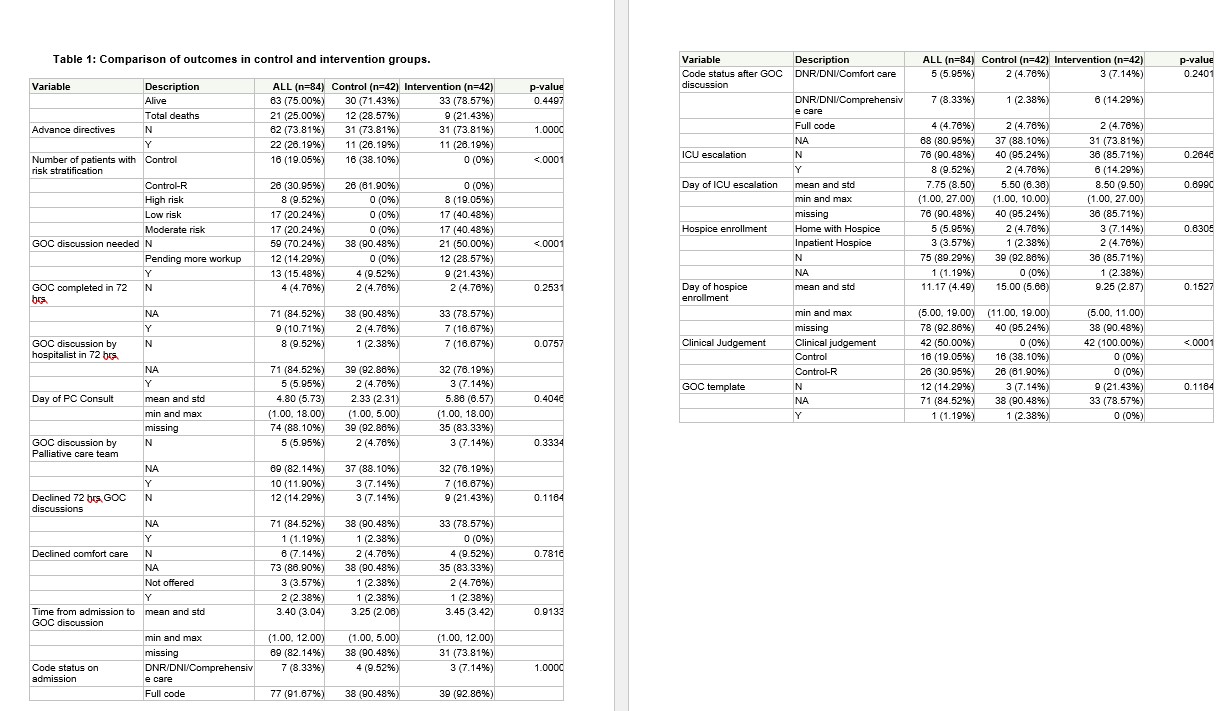
Methods: This is a non-randomized observational quality improvement pilot study with a waiver from our institutional review board. 84 patients who met the criteria for the risk of inpatient mortality ( risk score >-2.19) using the mortality prediction model were included. The primary hospitalist was notified of these patients on Day 2 of the hospitalization to trigger GOCD by day 3. Our main outcome was the percentage of patients in the intervention group who were agreed upon by the hospitalists that needed GOCD during that admission. Secondary outcomes included the percentage of GOCD completed within 72 hours, change in code status after the intervention, intensive care unit ( ICU) escalations, inpatient hospice length of stay, and discharge disposition. We also compared the mortality prediction of the hospitalist to the model’s performance. To confirm the validity of the model we compared mortality between the included and excluded patients in the pilot study.
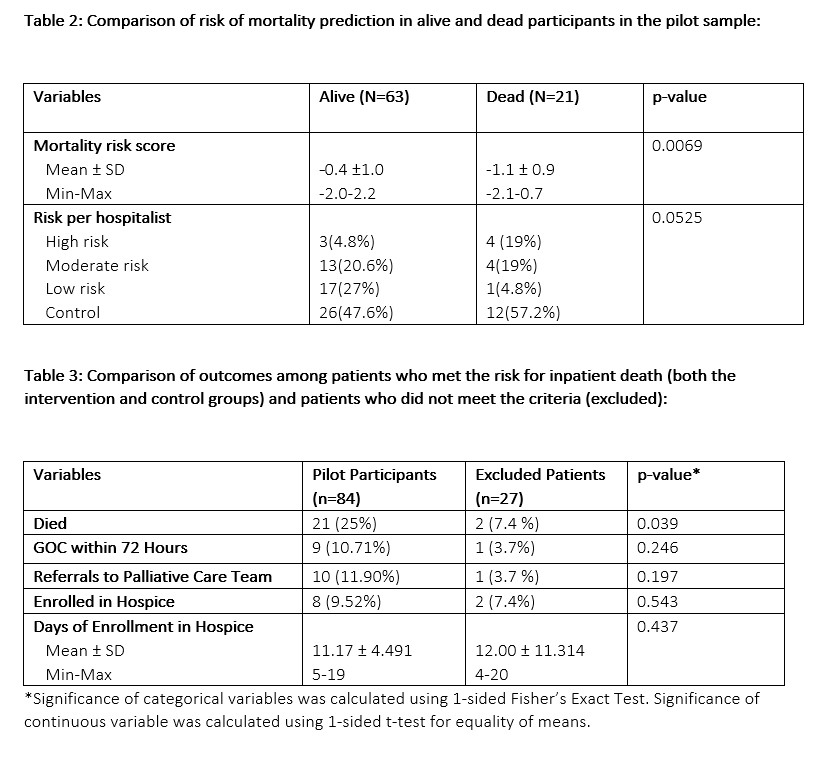
Results: The control and intervention periods included 12 weeks each and had 42 transferred patients in each group who met the modeled inpatient mortality cut-point trigger. 30-day inpatient mortality score was similar between groups with a mean (standard deviation) risk of -0.57 (1.06) in the control group and -0.55 (1.06) in the intervention group. All 42 screened patients in the intervention group were characterized as at risk for inpatient death by hospitalists. Hospitalists agreed that 9 patients ( 21.43%) in the intervention group needed GOCD vs 4 ( 9.52%) in the control group ( p< 0.001, Table 1). Although the small sample size precludes definitive conclusions ( Table 1), in the intervention group, we observed more GOCD were completed within 72 hrs. (16.67% vs 4.76%, p=0.2531) more patients agreed to GOCD ( 21.43% vs 7.14%, p=0.1164) or comfort care ( 9.52% vs 4.76%, p=0.7816), had a changed code status ( 21.43 % Vs 7.14%, p=0.2401), were enrolled into inpatient hospice ( 4.76% vs 2.38%, p=0.6305), discharged with home hospice ( 7.14% vs 4.76%, p=0.6305), and had an earlier average day of hospice enrollment ( 9.25 days vs 15 days, p=0.1527). Surprisingly, more ICU escalations occurred in the intervention group ( 14.29% vs 4.76%, p=0.2646) but they occurred later in the hospital course ( 8.50 days vs 5.5 days, p=0.6990). Inpatient mortality risk prediction ( Table 2) was statistically significant with the model (p=0.0069) as compared to the clinical judgment of the hospitalists ( p=0.0525). Patients who were included in the pilot study by meeting the risk threshold for inpatient death were significantly more likely to die than those who did not meet the threshold and were excluded from the study (Table 3, p=0.039).
Conclusions: Implementing an EHR-based mortality model to prompt early GOCD in the hospital course is feasible and may be a promising approach to improve end-of-life care. Despite the small sample size in our prospective pilot study, this model screened patients at high risk for inpatient death effectively and provided an opportunity for early GOCD. Larger randomized control trials are needed to determine its acceptability and association with significant patient outcomes.