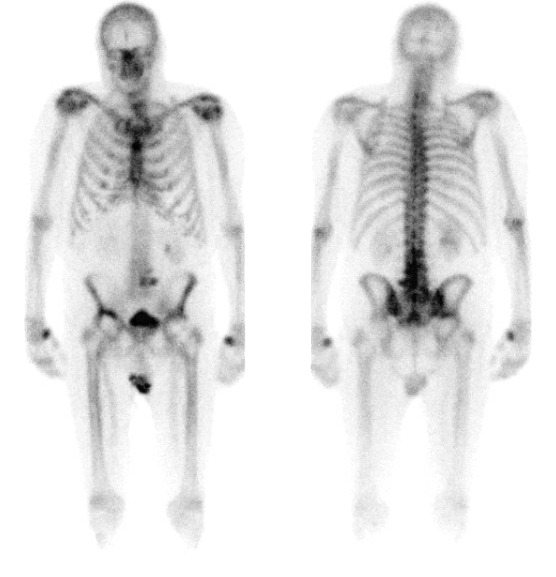
Case Presentation: A 79-year-old male with a past medical history of non-small cell lung cancer and squamous cell carcinoma of the left tonsil presented with right hip pain for the past couple of months. The pain had been progressively increasing and was associated with swelling around the joint. The patient had a bilateral hip replacement in 1994 for arthritis. Hip-X ray was done which showed asymmetric acetabular cup loosening. The patient’s annual bone scan demonstrated moderate peri-prosthetic increased activity corresponding to asymmetric superior acetabular sclerosis, otherwise mild diffuse bilateral hip peri-protheses uptake was unremarkable. Effusion surrounding the hip joint was found on examination, which was subsequently tapped. Synovial fluid showed increased Plasma cells which warranted a workup for Multiple Myeloma (MM). SPEP showed M spike at 3.07, Ig A of 3610 and K/L 167.25. Bone marrow biopsy showed increased plasma cells at 50-60% of cellular elements by CD138 Immunohistochemistry. The plasma cells were kappa light chain restricted by in situ hybridization and by flow cytometric analysis. These findings in addition to a serum-free light chain ratio >100 completed the WHO criteria for the diagnosis of MM. In light of the diagnosis, the patient was started on appropriate treatment.
Discussion: Multiple myeloma (MM) is a result of abnormal plasma cell proliferation in the bone marrow and accounts for 10% of the hematological malignancies. Joint involvement in myeloma is typically an oligoarthritis or a polyarticular rheumatoid-like pattern, though individuals with myeloma are at greater risk of both septic arthritis and gouty arthritis. The direct tumor invasion of the joint has been identified in other primary hematological malignancies, however, it is extremely rare in MM.Studies have shown that hip replacement does not increase overall cancer risk in patients, although there have been few reports of rare malignancies near-total hip prostheses. Commonly reported radiological periprosthetic lucency is a well-recognized sign suggestive of aseptic loosening of or infection around the prosthesis. In one study the overall prevalence of periprosthetic lucency was 5.02%. The prevalence of metastases or multiple myeloma near a hip prosthesis was 1.54%; however, each of these patients had a known prior diagnosis of bone metastases, multiple myeloma, or primary bone malignancy. No primary malignancy or metastasis was discovered initially as an osteolytic lesion near the hip prosthesis. This case is distinctive as MM was diagnosed as primary malignancy at the hip prosthetics and also the diagnosis was made on the basis of synovial fluid analysis.
Conclusions: A primary malignancy or metastasis presenting as periprosthetic lucency is an extremely rare occurrence. This case emphasizes the significance of evaluating the cause for loose prosthesis and analyzing the synovial fluid especially in patients with a history of previous malignancies.