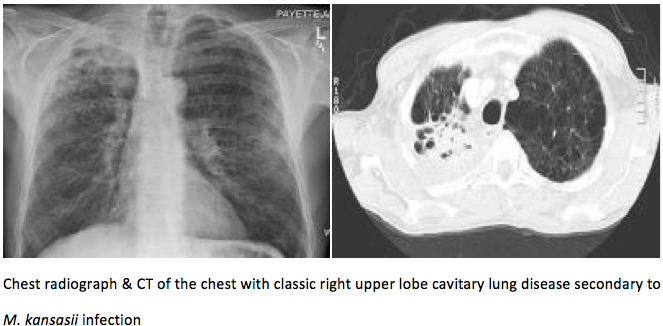
Case Presentation: A 57 year old male with past medical history of COPD and schizophrenia presented with complaints of shortness of breath. The patient was discharged from a different hospital a day prior to the admission. Patient had to be intubated secondary to hypercapnic respiratory failure and was sent to the ICU. He remained intubated for five days. Chest X-ray showed mediastinal shift to the right. A cavitary lesion was seen in the right upper thorax, a nodular soft tissue density was also seen with some speculation that appeared to be a mild infiltrate. This was followed up with a CT scan of the chest that suggested an old infectious process and COPD. The patient underwent further serological workup and this revealed neutrophilia but no leukocytosis, HIV serology was negative and Quantiferon gold test was indeterminate. Sputum culture and blind bronchoalveolar lavage (BAL) grew oronasal flora. The outside hospital records were obtained and these indicated that the patient had undergone a bronchoscopy and the right upper lobe cavitary lesion had grown Mycobacterium kansasii (M. kansasii). The patient was started on Rifampin, Isoniazid, Pyridoxine and Ethambutol therapy. The patient was eventually discharged home with home oxygen.
Discussion: Mycobacteria other than M. tuberculosis and M. leprae are generally free-living organisms that are ubiquitous. They have been found in tap water, soil, domestic and wild animals, milk, and food products. They can also inhabit body surfaces or secretions without causing disease. Thus, occasional isolates of nontuberculous mycobacteria (NTM) were largely considered contaminants. However, the importance of NTM in human disease has become increasingly evident lately. M. kansasii is an acid-fast bacillus that is readily recognized based on its characteristic photochromogenicity, which produces a yellow pigment when exposed to light. The major risk factor for pulmonary M. kansasii infection is COPD. According to the 2007 ATS/IDSA guidelines, the general diagnostic criteria for all NTM pulmonary infections include clinical and radiological criteria. The criterion includes pulmonary symptoms with nodular or cavitary opacities on chest radiography or a HRCT scan that shows multifocal bronchiectasis with multiple small nodules. In terms of the microbiologic criteria one of the following is required: positive culture results from at least 2 separate expectorated sputum samples, or a positive culture from endotracheal sample, BAL or a lung biopsy. Nucleic acid probes and polymerase chain reaction are useful for early identification. Treatment consists of a three-drug combination that consists of Isoniazid 300 mg daily, Rifampin 600 mg daily and Ethambutol 15 mg/kg per day. Duration of treatment is recommended to be 12 months with negative cultures.
Conclusions: This case illustrates a fairly typical presentation of M. kansasii. Clinical suspicion and early recognition are critical as prompt initiation of therapy aids in preventing significant morbidity.