Case Presentation: A 30-year-old man with sickle cell anemia presented to the ED with pain in his left hip similar to prior vasooclussive crisis (VOC). There was no identifiable trigger and his review of symptoms was negative. Past medical history included sickle cell anemia complicated by acute chest syndrome (ACS), avascular necrosis of the right hip and immune-related thrombocytopenia. He had never smoked and reported no alcohol or IV drug use. Outpatient medicines included morphine SR, hydromorphone and folic acid. On hospital day 2, he developed tachycardia, hypotension and hypoxia requiring ICU care. He was in no distress but had new right lower lobe crackles. CT pulmonary embolism protocol was negative for PE but revealed multifocal opacities, severely enlarged mediastinal lymph nodes, and severe right-sided ventricular and pulmonary artery enlargement. He underwent emergent exchange transfusion for presumed acute chest syndrome. On hospital day 3, he expired from hypoxic PEA arrest. Autopsy revealed heavy lungs (right: 1115 gm; left 1137 gm. Normal ~500 gm) with intravascular talcosis and associated granulomatosis of pulmonary arterioles with multiple foci of pulmonary hemorrhage (up to 2.0 cm) diagnostic of pulmonary talc granulomatosis.
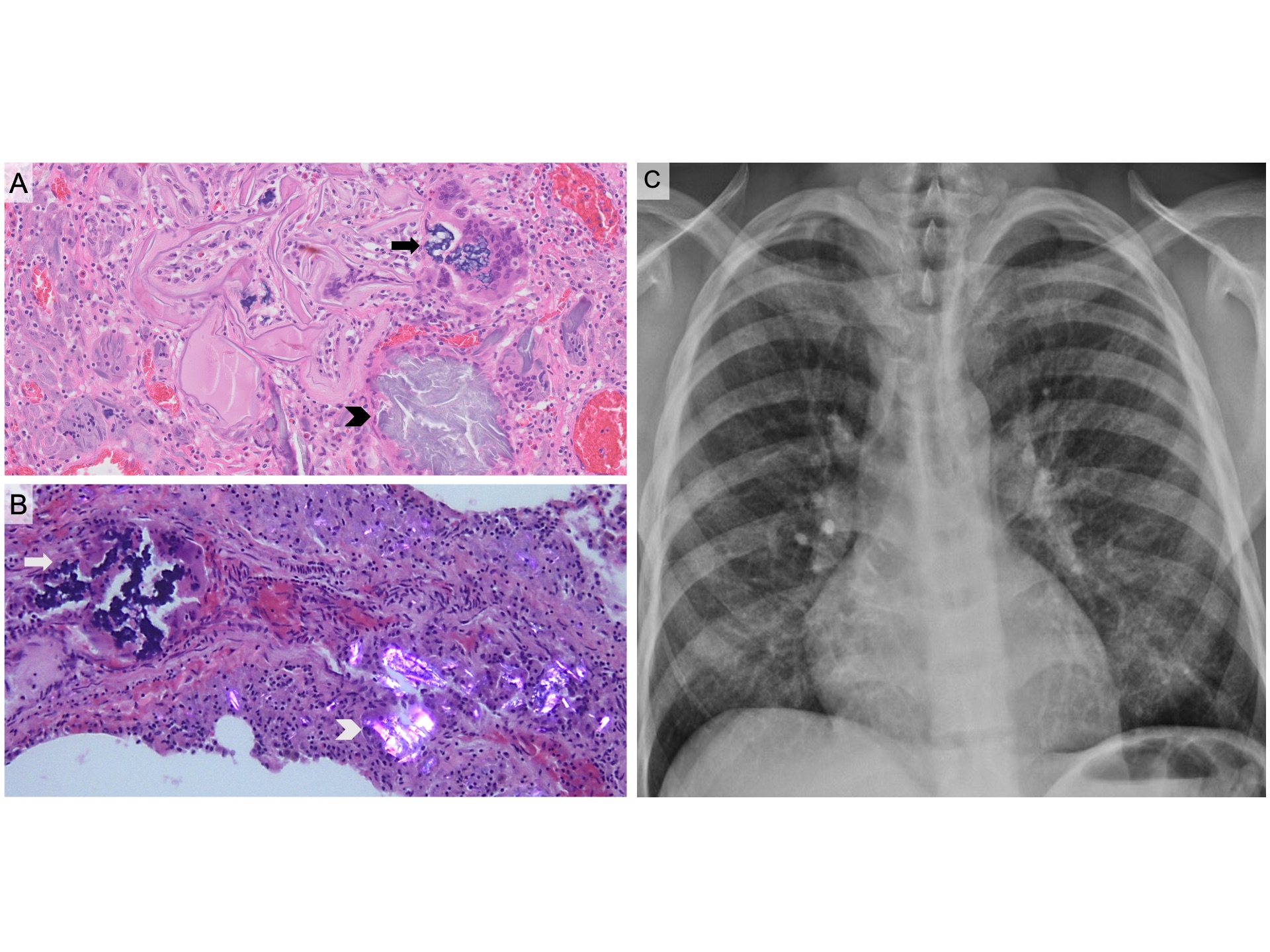
Discussion: Our patient suffered PEA arrest due to acute pulmonary microhemorrhages secondary to pulmonary talc granulomatosis (PTG) and associated vascular inflammation and interstitial fibrosis diagnosed on autopsy. PTG is most commonly caused by occupational or incidental inhalation of talc, a hydrated magnesium silicate mineral found in cosmetic products.[1] PTG may result from deposition of pill excipients, such as microcrystalline cellulose (MCC)(Panel B, polarized H&E, arrowhead) and crospovidone (Panel B, arrow), following intravenous injection of crushed pills.[2-4] Our patient was noted to self-administer crushed PO medicines through his port-a-cath during a prior admission. The duration of our patient’s behavior is unclear, however the extent of vascular and interstitial inflammation and fibrosis on autopsy suggest a chronic nature. Our patient had a micronodular pattern chest radiography noted 5 years prior to admission consistent with early findings of PTG (Panel C).[2, 5, 6] Intravenous injection of crushed PO medicines represents a morbid and under-diagnosed behavior in the setting of drug use disorder and chronic pain. Little to no epidemiologic data is available on this behavior. Increased awareness in the inpatient setting is critical as patients frequently have IV access and access to home medications. Self-injection of foreign material into peripheral IVs is associated with infectious complications including bacteremia for which our patient had been diagnosed.[7, 8] The chronicity of our patient’s behavior highlights the lack of awareness of this pathology and missed opportunities for appropriate behavioral intervention and prevention.
Conclusions: Pulmonary talc granulomatosis as a result of intravenous injection of crushed PO medicines is a rare complication of drug use disorder. Increased awareness of this behavior may lead to early detection, appropriate behavioral intervention and prevention of life-threatening sequelae.