Background: Excess alarms cause a phenomenon, known as alarm fatigue, in which medical providers become desensitized to constant noise emitted from monitors & fail to notice or react to alarms which can lead to patient safety concerns. With the acceleration of remote monitoring & monitoring hubs, it is critical to minimize unactionable alarms and prevent alarm fatigue.
Purpose: The purpose of our project was to create a multi-step approach to minimize unactionable alarms within our hospital system and in turn, prevent alarm fatigue amongst front line providers.
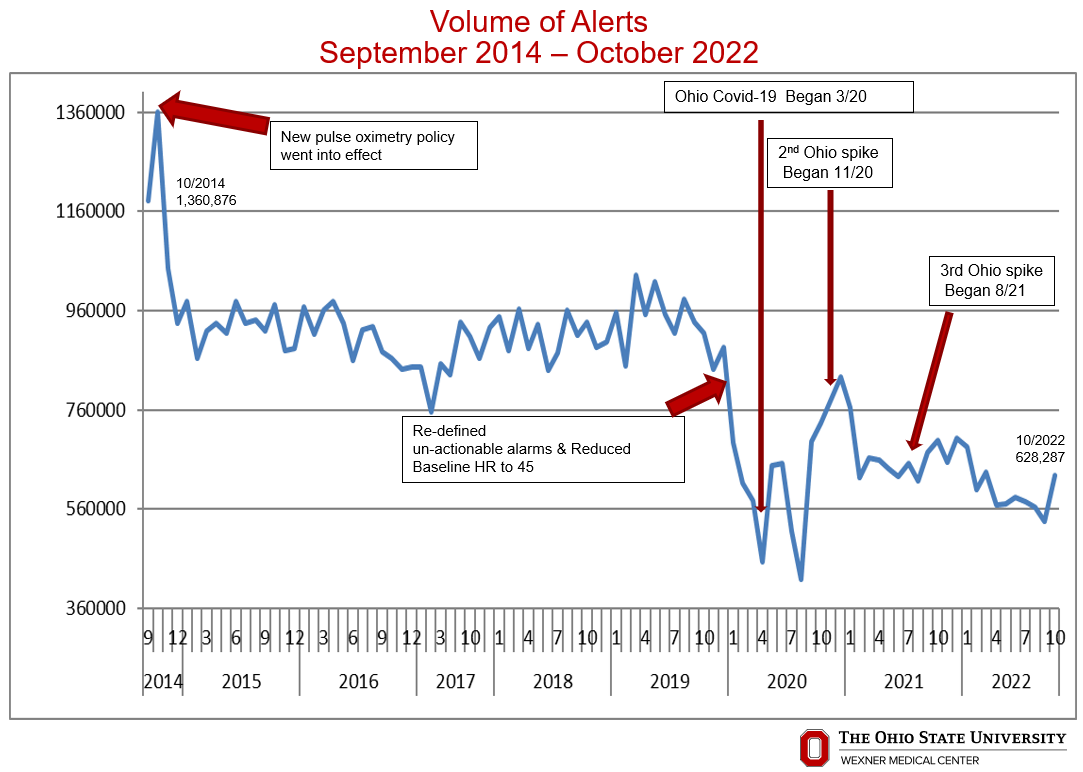
Description: Utilizing DMAIC methodology, we evaluated our institutions alarms, policies, & equipment manufacturer recommendations. Next, we reviewed internal data and identified pulse oximetry alarms as our largest contributor to alarms, creating 60-65% of our institution’s total alarms. Our pulse oximetry alarms were initially set to alarm when a patient’s oxygen saturation fell below 92%. This was not commonly adjusted by providers despite the patient’s clinical condition. Therefore, we reviewed available literature to identify best practices & changed our institutional pulse oximetry alarm threshold to 88%, with the caveat providers could always increase the threshold for specific clinical conditions (example – reperfusion after cerebral thrombectomy). This change was made in October of 2014 and resulted in a decrease in alarms from 1.36 million alarms per month to 914,261 alarms per month by October 2019. This represents a sustained reduction of 33% in unactionable alarms despite hospital growth & increased number of hospitalized patients. In 2019, we again utilized a multidisciplinary team and DMAIC methodology to repeat a similar process as noted for pulse oximetry, for cardiac monitoring. In addition we partnered with General Electric (GE), our cardiac monitor manufacturer, to review industry alarm nomenclature, policy and recommendations. Partnering with GE, we were able to streamline nomenclature to remove redundant audible alarms. Specifically we were able remove audible alarms from nomenclature associated with tachycardia, SV tachycardia, and bradycardia, as they alarmed with other names as well. In 2019, we also utilized DMAIC methodology to run pilots on multiple units in our hospital system including the heart hospital, cancer center, and university hospital to standardize audible heart rate alarm limits. Based on our pilots, we were able to reduce the heart rate lower limit from manufacturer standard of 50 beats per minute to 45 beats per minute & increase the upper limit to 130 beat per minute. These changes did not result in any increased patient harm or safety events. Thus in November 2019, we implemented the new heart rate limits across our institution. These changes resulted in a decrease in alarms from 800,000 alarms per month in November of 2019 to 628,287 alarms per month by October 2022. This represents an additional reduction of about 20% in unactionable alarms.
Conclusions: Utilizing DMAIC methodology, partnering with physiologic monitoring manufacturers and frontline providers, we have been able to reduce audible alarm noise across our institution by close to 50% over the past decade. These results sustained through the COVID pandemic despite the increased usage of physiologic monitoring. Lessons learned from this process will be paramount to reduce alarm fatigue as hospitals continue to implement remote monitoring & monitoring hubs.