Background: The incidence of Opioid Use Disorder (OUD) is rising around the world with nearly 27 million people living with OUD globally and over 100,000 opioid overdose deaths each year. The Society of Hospital Medicine recently released a consensus statement for management of patients with OUD admitted to the hospital. This statement included recommendations for patients to be offered buprenorphine or methadone as first-line agents to treat opioid withdrawal and OUD, for hospitalists to obtain an X waiver to prescribe buprenorphine at hospital discharge and to connect patients with outpatient care for ongoing medication for OUD (MOUD). Acute hospitalizations provide a key opportunity for healthcare providers to intervene, initiate treatment and provide ongoing resources for patients with OUD.
Purpose: To implement interventions including physician, advanced practice provider, nursing, and pharmacist education, standardized treatment protocols, and outpatient treatment resources to improve care for patients with opioid withdrawal and OUD in the hospital.
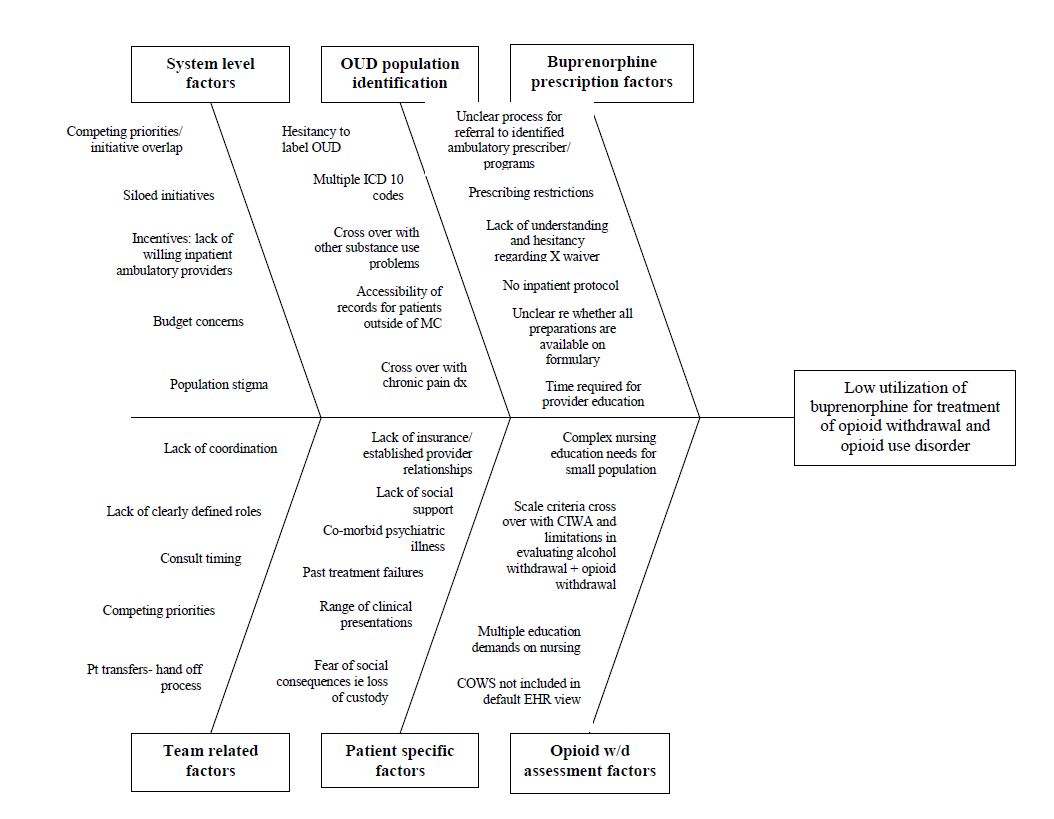
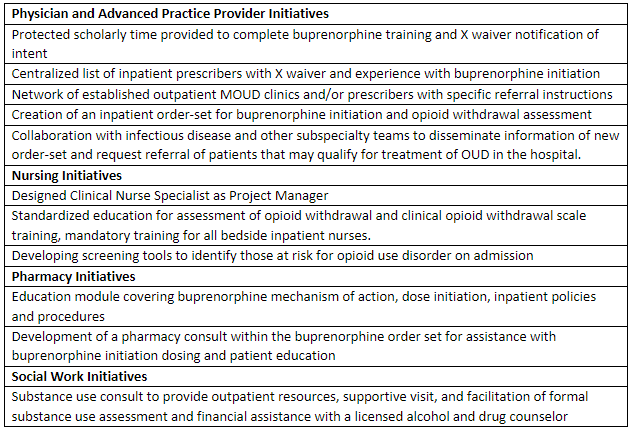
Description: Our intervention began with the creation of a multidisciplinary workgroup including inpatient and outpatient physicians, advanced practice providers, as well as stakeholders from pharmacy, nursing, social work, and informatics. Baseline data suggested significant underutilization of buprenorphine for the treatment of opioid withdrawal in the hospital in the year prior to creation of the workgroup. Stakeholder feedback identified barriers to overcome including need for a standardized dosing protocol, improved education for physicians and advanced practice providers, access to expert consultation for complex cases, improved nursing familiarity and training for opioid withdrawal assessment, barriers to receiving X waiver, limited awareness of outpatient resources, and others (Figure 1). With this feedback in mind, we implemented a multipronged approach to improve the care of patients with OUD in the hospital (Figure 2). We have developed new educational tools for assessment of opioid withdrawal using the Clinical Opioid Withdrawal Scale (COWS) that will roll out to all inpatient bedside nurses in the next calendar year. New pharmacist, physician, and patient educational tools are also in development to launch on the same timeline. After implementation of the described interventions (Figure 2) we will re-evaluate the percentage of patients presenting with opioid withdrawal that are initiated on MOUD during their inpatient stay.
Conclusions: Patients presenting with OUD represent a vulnerable and often marginalized patient population. Through the implementation of a multidisciplinary approach, we hope to optimize the care of these patients, bridging the gaps in current clinical practice to enhance the availability of potentially lifesaving medication treatment with buprenorphine.