Background: High-quality medication reconciliation is key to reducing medication errors during care transitions. This concept is of paramount importance to Veterans living in rural areas due to less access to clinical pharmacy services. We adapted MARQUIS (Multicenter Medication Reconciliation Quality Improvement Study), in which hospitalists mentored teams in implementation of best practices for inpatient medication reconciliation, to the VA context. We then implemented and evaluated R-VA-MARQUIS in 3 rural VA Medical Centers as a multi-site quality improvement project.
Methods: Principal investigators conducted site visits to generate recommendations from the best practices toolkit and mentored improvement groups through implementation. Trained project pharmacists or nurses completed data collection from January to September 2015 by performing a best possible medication history and documenting unintended discrepancies with the primary team’s history, admission and discharge orders. Mean discrepancies were compared pre- and post-intervention for the sites using Wilcoxon rank sum tests. We compared data from all sites pre- and post-intervention using logistic regression with an outcome of >1 vs. 0-1 total discrepancies adjusted for age and admission in the prior year. The cutoff was selected because prior studies have demonstrated that highest quality reconciliation reduces the mean rate to one discrepancy per patient.
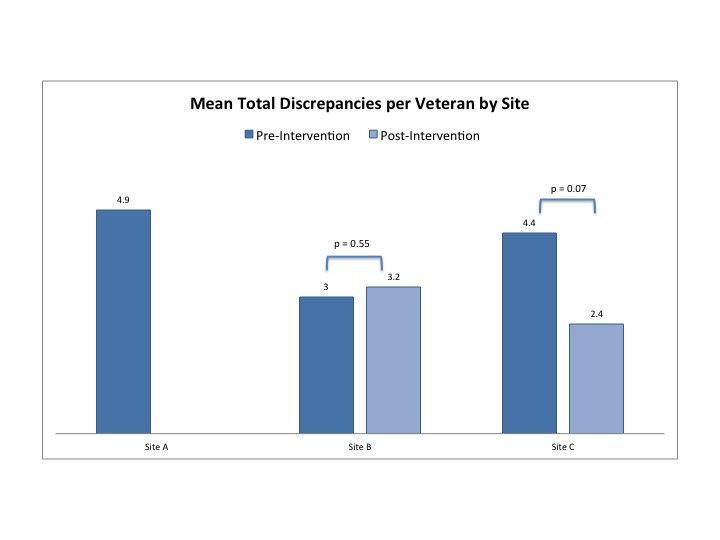
Results: There were 301 Veterans hospitalized at 3 sites. Veterans were 94% male and 86% white with a mean age of 68 (SD 11.7). Median length of stay was 2 days (IQR 2,4), and 58% of the Veterans had been hospitalized in the prior year. Site populations were similar, including mean number of medications per Veteran. Site A did not implement any toolkit interventions. Site B implemented interventions on admission reconciliation, and Site C implemented interventions on discharge reconciliation. Mean total discrepancies varied by site (Figure 1). Site A had a baseline mean of 4.9 total discrepancies per Veteran. Site B had an increase in mean total discrepancies from 3 to 3.3 after intervention. Site C reduced mean discrepancies from 4.2 to 2.2. In adjusted logistic regression comparing pre- to post- intervention, the odds of having more than one discrepancy decreased (OR=0.44, CI 0.25, 0.77, p<0.01).
Conclusions: After the first year, implementation of R-VA-MARQUIS was associated with reduced discrepancies. While sample size limited the ability to draw statistical conclusions about individual intervention effects, analysis will continue in the second year of the project. The early results of R-VA-MARQUIS support that providing smaller, rural VAMCs with tools and subject-matter mentorship may promote high quality care for Veterans.