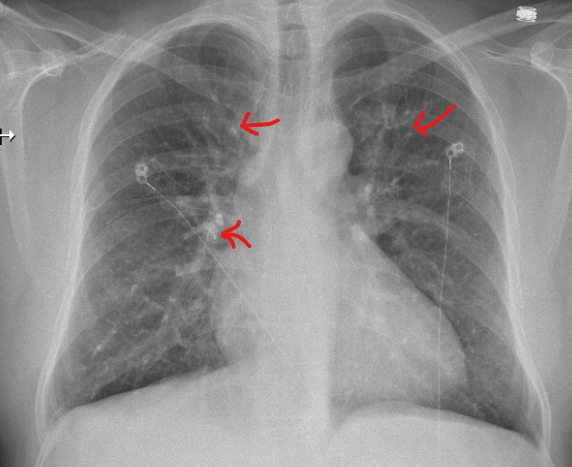
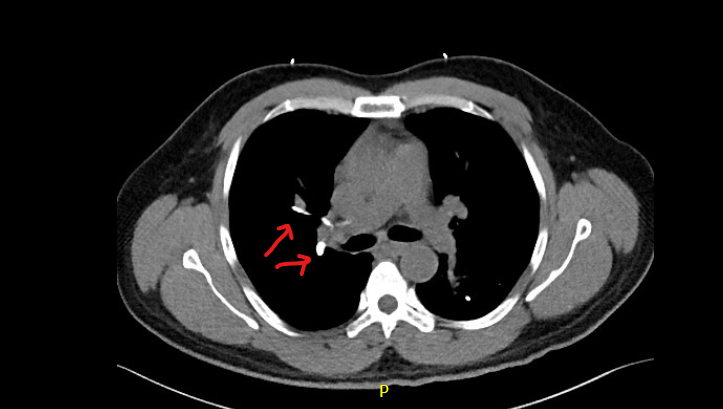
Case Presentation: A 50-year-old man with known liver cirrhosis secondary to schistosomiasis transferred to our facility for the management of large gastric fundus varices seen on CT abdomen and pelvis. Esophagogastroduodenoscopy (EGD) showed grade I esophageal varices and isolated large gastric fundal varix without bleeding and signs of portal hypertensive gastropathy. Patient was not deemed a candidate for Transjugular Intrahepatic Portosystemic Shunt (TIPSS) due to history of portal vein thrombosis. Given the size of gastric varix and high risk of spontaneous bleeding, we decided to pursue with intra-variceal (gastric) injection of N-butyl-2-cyanoacrylate (Histoacryl) glue. Shortly after the procedure, patient developed tachypnea and shortness of breath with oxygen desaturation to 91% requiring 2 L of supplemental oxygen via nasal canula. Other vitals were T: 37.9°C (100.2°F), RR 29 bpm, HR 94 bpm, BP:137/58 mmHg. Pertinent labs included WBC: 12.89 x 109/L, Hemoglobin 89 g/L, Troponin-T: 0.019 µg/L (Normal reference <0.06 μg/L), NT-Pro BNP: 59.0 ng/L (Normal reference <121 ng/L). A stat chest x-ray revealed multiple small radiopaque opacities in both lungs suggestive of possible foreign body emboli. ECG showed normal sinus rhythm with no signs of right heart strain or arrhythmia. Subsequently, a Computed Tomography Angiogram (CTA) chest revealed high density embolic material and filling defects at the bifurcation of the right upper and lower lobe pulmonary arteries, within the segmental branches; right apical, anterior right upper lobe, right proximal lateral middle lobe, left apical; and multiple sub-segmental filling defects bilaterally. Patient symptomatically improved, remained hemodynamically stable, white count normalized and weaned off oxygen within 48 hours, while on conservative management. He was discharged and had an uneventful follow up with pulmonary team at 1 week.
Discussion: N-butyl-2-cyanoacrylate (Histoacryl) glue injection sclerotherapy is highly effective for the treatment of gastric varices. Complications include glue embolization, mesenteric or portal vein thrombosis, sepsis, local ulceration or fistula formation. Histoacryl pulmonary embolism is not uncommon with reported incidence of up to 4%. Risk increase with size of varices, injecting large volume of polymerizing agent (more than 1 ml), slow injection, and amount of distilled water flushes post injection. Embolization is thought to be due to delay in polymerization leading to migration of the glue material beyond the varices through the gastro-renal veins and spleno-renal to the inferior vena cava and systemic circulation. Embolism of injected glue material has been reported to occur a few days after the procedure (10 days per one case report). Majority of the glue pulmonary embolism patients are generally stable and return to baseline pulmonary function, but close monitoring is recommended to observe for serious complications such as ventricular arrhythmia and/or cardiorespiratory failure, which has been reported in the literature. Treatment is mainly supportive. Anticoagulation or thrombolysis is not recommended. Long term sequalae may include pulmonary fibrosis, pulmonary hypertension and restrictive lung disease.
Conclusions: Acute Pulmonary Embolism post gastric variceal glue (histoacryl) injection should be suspected in symptomatic patients. Interestingly, a plain chest x-ray can be diagnostic owing to the radio-opaque glue in the pulmonary vasculature.