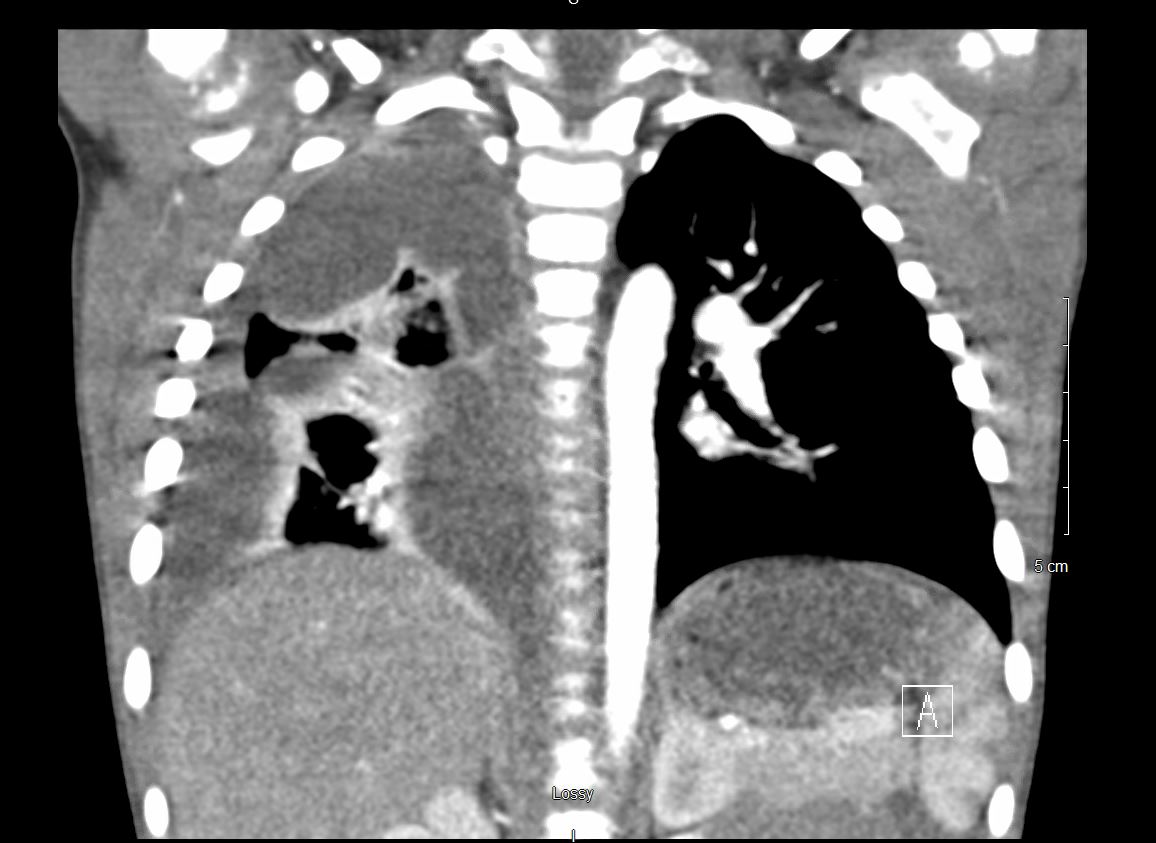
Case Presentation: A 2-year-old male, with no significant past medical history, presented to a tertiary children’s hospital with a 3-day history of fever and cough. Associated symptoms included chills, fatigue, and acute onset shortness of breath. Parents denied recent travel or sick contacts. Initial exam was significant for decreased breath sounds in the right lower lung field and bilateral cervical lymphadenopathy. Chest x-ray demonstrated right sided multi-lobar pneumonia with a parapneumonic effusion. Follow up CT (Figure 1 and 2) demonstrated a large, right-sided empyema without necrotizing pneumonia or cavitary changes. Patient underwent video-assisted thoracoscopy with pulmonary decortication and pleural debridement on hospital day 2. Bacterial, fungal, and mycobacterial cultures of the pleural fluid were obtained. However, due to concern for potential low yield from pre-treated cultures and continued febrile state while on appropriate antibiotics, a universal bacterial PCR was also obtained. On hospital day 6, the universal bacterial PCR was positive for Mycobacterium Tuberculosis. Given this unexpected finding, further work-up was obtained including IGRA and mycobacterial smears and cultures of gastric aspirates. These ultimately resulted as positive. Following infectious disease consult, the patient was placed on 4-drug therapy with rifampin, isoniazid, pyrazinamide, and ethambutol to complete a 12-month course.
Discussion: While uncommon in the United States, tuberculosis (TB) affects approximately 10 million people globally each year with 10% of cases occurring in children (1). The primary manifestation in infants is shortness of breath with a nonproductive cough while older children typically demonstrate classic symptoms including weight loss, hemoptysis, and fever (2). While pulmonary empyema secondary to TB infection has been described in adults, these typically preceded introduction of modern antimicrobial therapy (3). Upon review, there is little available literature regarding pulmonary empyema secondary to TB infection in children. One clue to the etiologic agent, in this child’s case, was the absence of necrosis or significant parenchymal involvement. Similar CT findings have been described in other cases (4). With this in mind, if a child is hospitalized for pneumonia and the imaging is not consistent with parenchymal involvement, then TB should be considered and an investigation for risk factors and further work up should be pursued.
Conclusions: Pulmonary empyema secondary to tuberculosis is uncommon in the pediatric population. Healthcare providers should consider tuberculosis in the differential for any child with a clinical diagnosis of pneumonia, failure to respond to empiric antimicrobial therapy, and imaging findings with evidence of pleural effusion without parenchymal involvement.