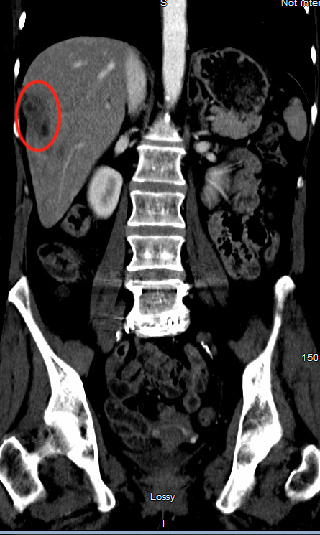
Case Presentation: Case of 53 years old female with a past medical history of rheumatoid arthritis, coronary artery disease and peripheral vascular disease who presented with worsening postprandial right upper quadrant abdominal pain. Pain was described as intermittent, sharp, and stabbing. The patient also reported a 20-30 pounds’ unintentional weight loss over 6 months and food aversion secondary to abdominal pain. Physical exam was notable for right upper quadrant abdominal pain upon palpation and stable vital signs. Labs were unremarkable. CT abdomen and pelvis was significant for new areas of hypodensity within the liver, high-grade stenosis of the proximal superior mesenteric artery (SMA) and a replaced common hepatic artery arising distal to the SMA stenosis. The new areas of hypodensity were concerning for areas of infarct given this patient’s history of vascular disease versus hepatic abscess. Interventional Radiology was consulted and an SMA arteriography was performed. The SMA arteriography confirmed the severe proximal SMA stenosis which was subsequently treated with a 6×24 mm stent placement. After the procedure, the patient experienced significant clinical improvement with adequate oral intake and decreased abdominal pain.
Discussion: The common hepatic artery (CHA) is one of the final branches of the celiac artery and it supplies blood to the liver, pylorus, pancreas, and duodenum. Anatomical variations of the common hepatic artery are rare. The replaced common hepatic artery (RCHA) is a rare anatomic variation in which the CHA arises from a different source other than the celiac trunk. The most common variation arises from the superior mesenteric artery. The RCHA is mostly asymptomatic and detected incidentally on imaging. However, when gastrointestinal symptoms of unclear etiology are present, such as in this case, high clinical suspicion for vascular variations and stenosis should be considered. The SMA and CHA are major arterial suppliers of the liver and pancreaticobiliary system. The absence of hepatic arterial blood flow can lead to liver ischemia and necrosis. Most cases of severe SMA stenosis present similarly to chronic mesenteric ischemia (CMI) with abdominal pain, weight loss, and food aversion. CMI is characterized by stenosis or occlusion of at least two of the three mesenteric arteries. Revascularization is the mainstay of treatment. To our knowledge, a replaced common hepatic artery presenting as chronic right upper quadrant abdominal pain due to a hepatic infarct has not been presented in the literature. Awareness of such anatomical variations are clinically relevant to avoid significant surgical complications and to aid in the correct diagnosis and management.
Conclusions: This case highlights the importance of being aware of the normal vascular anatomy of the liver as well as its possible variations. Thorough evaluation of the liver vascular anatomy through standard imaging modalities is crucial when the clinical presentation is unclear.