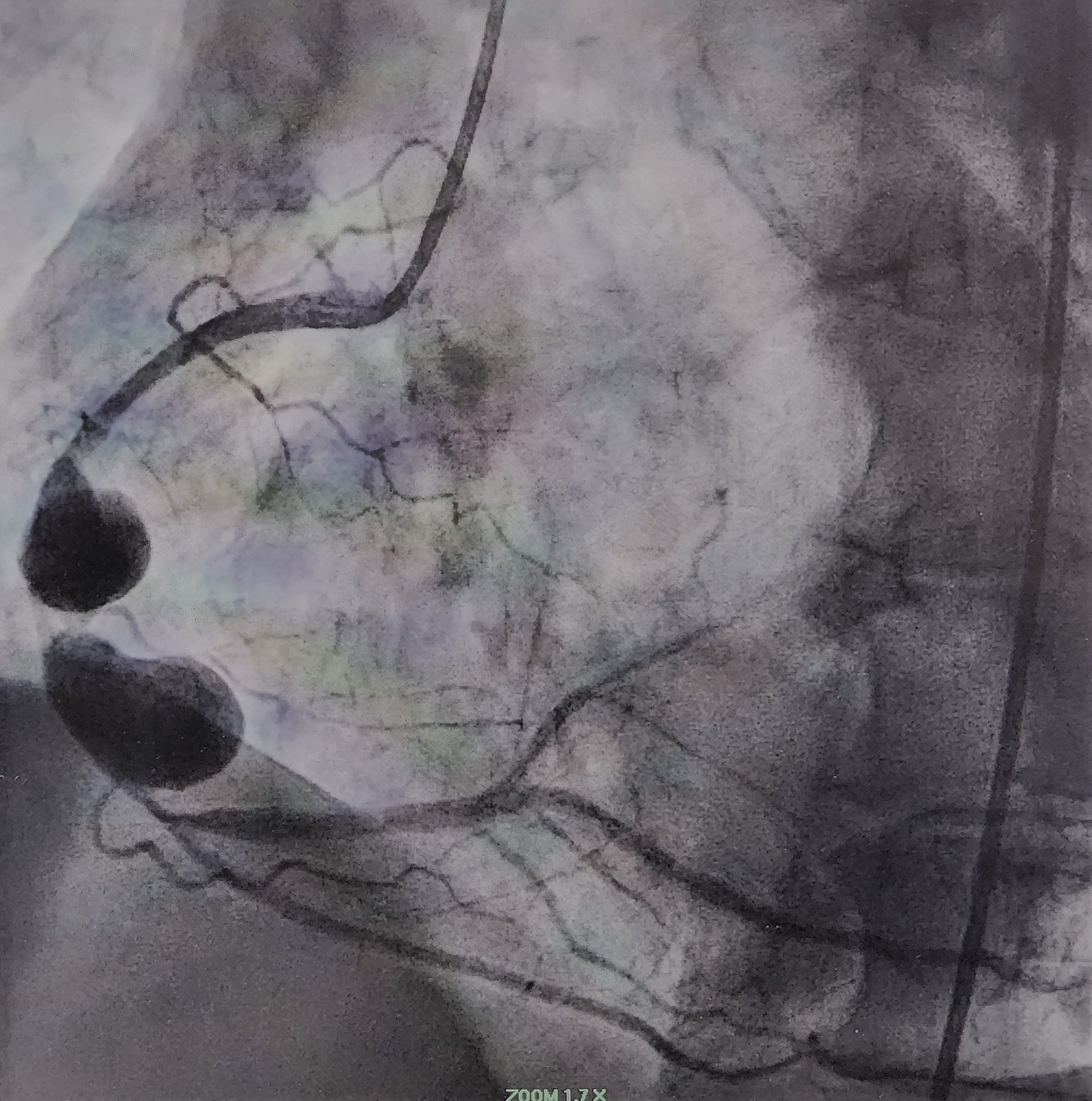
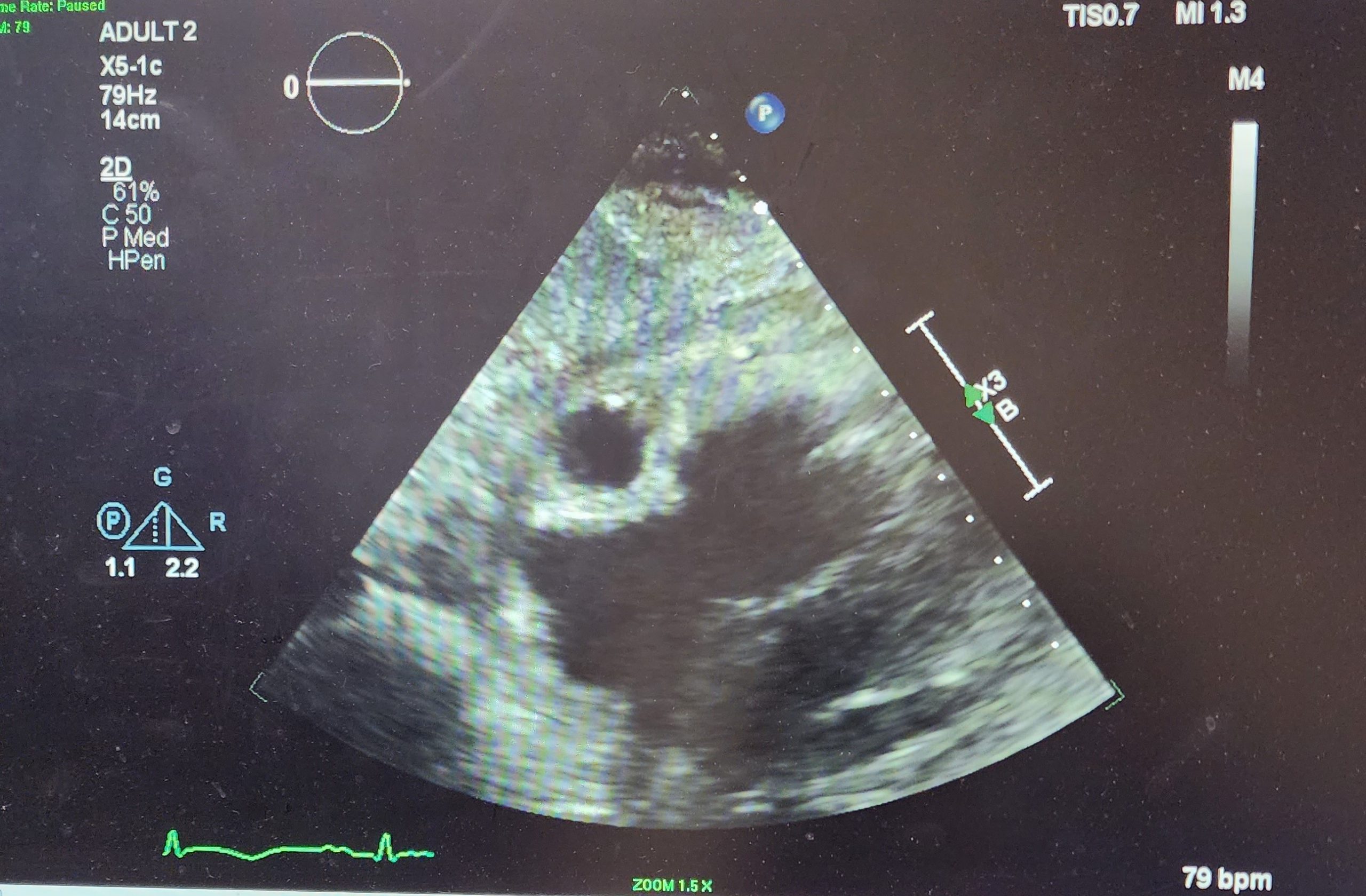
Case Presentation: A 70-year-old woman with a past medical history of CKD stage IV, nephrolithiasis, Crohn’s disease presented to the Emergency department for two weeks of nausea, anorexia, dehydration, fever, chills, lightheadedness with right upper quadrant pain. Upon admission the patient was in shock, differentials included septic vs cardiogenic. BNP was 354 pg/mL and troponin I was persistently elevated. Initial CBC showed a leukocytosis of 29.1. The patient was promptly placed on fluids, antibiotics and vasopressors. An echocardiogram was performed revealing an ejection fraction of 25-30%, akinetic apex and basal portions, mild mitral and tricuspid regurgitation, RVSP of 28 mmHg, and an echolucent structure noted within the right sided pericardial effusion. Initial EKG was relatively nonsignificant, and the patient was treated as a NSTEMI. The following day a repeat EKG showed significant ST elevation in the inferior and posterior leads prompting an order for coronary angiogram and a heparin drip. The angiogram revealed two large coronary artery aneurysms involving the mid segment of the RCA. Both aneurysms measured about 4 x 5 centimeters in length with moderate stenosis between them in the shaft of the RCA. Angiogram also revealed 40% narrowing in mid segment of LAD. Throughout the patient’s hospitalization there was no reported chest pain.
Discussion: Most coronary artery aneurysms (CAA) develop due to atherosclerosis (~50%) but other etiologies such as Kawasaki and polyarteritis nodosa can also lead to CAAs. The pathophysiology of coronary artery aneurysms can be divided in to two major categories which follow similar mechanism. Atherosclerotic damage is usually caused by oxidized LDL and pro inflammatory cytokines leading to ECM matrix remodeling and vessel wall damage leading to weakening and thinning of the vessel wall and eventual ballooning. Kawasaki and other vasculitis usually share similar pathophysiology of inflammation and vessel damage leading to the aneurysm. In this case, our patient most likely had atherosclerosis that caused the most distal aneurysm followed by a thrombus formation leading to the sequential second aneurysm and myocardial infarction. Though most cases are usually asymptomatic, it is important to understand possible complications such as myocardial infarction, tamponade, or compression of other cardiac chambers.
Conclusions: Coronary artery aneurysm (CAA) is a rare medical condition with incidence of 0.3 to 5%, and giant CAA’s defined as >8mm in diameter are even rarer with an incidence of 0.02%. Cases of multiple aneurysms occurring simultaneously are isolated and even fewer. Underlying causes of coronary artery aneurysms include atherosclerosis, Kawasaki disease, Takayasu arteritis, iatrogenic post PCI, congenital heart defects and connective tissue disorders such as Marfan Syndrome. CAA can be initially diagnosed by echocardiogram, CT or MRI, and is confirmed by coronary angiography. Treatment options include medications management, percutaneous coronary angiography, and surgical repair. The patient underwent cardiac catheterization which revealed 2 large aneurysms in the mid segment of the Right Coronary Artery (RCA) both measuring about 4 cm x 4 mm x 5 cm in diameter. This patient’s distal CAA was most likely the result of longstanding atherosclerosis, whereas her proximal CAA was likely a sequela of thrombus formation occurring in the distal aneurysm.