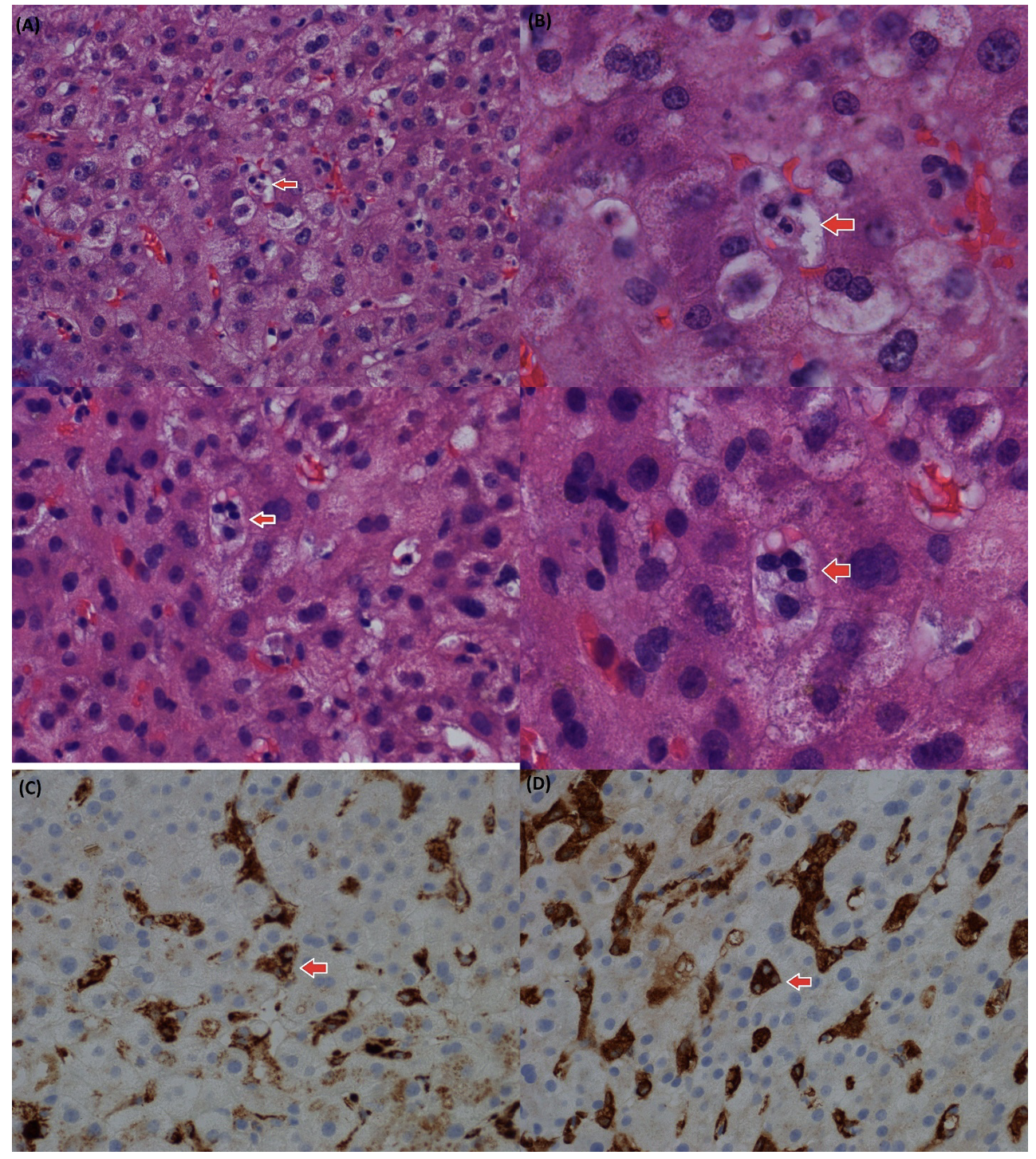
Case Presentation: An 18-year-old female with no significant medical history presented to the hospital with diffuse abdominal pain and jaundice for 2 weeks, associated with nausea, non-bloody vomiting, and subjective fevers. The patient was treated for exudative tonsilitis 2 weeks earlier and had taken 6 grams of acetaminophen over 48 hours before presentation to the hospital. On initial evaluation, vitals showed a fever of 38.8 °C, stable blood pressure, tachycardia, and tachypnoea. Physical examination revealed jaundice with scleral icterus and the right upper quadrant abdominal tenderness. Laboratory workup showed pancytopenia with hemoglobin 11.6 g/dL, white blood cell 1.8 x10^9/L, Platelet 43000 x10^9/L, and elevated liver function test. A Computed tomography scan of the abdomen and pelvis without contrast showed hepatosplenomegaly. She was admitted for sepsis and started on empiric antibiotics. Blood cultures were ordered. Hematology-Oncology, Infectious disease, and Hepatology were consulted. A broad spectrum of viral serology and autoimmune workups were ordered, showing positive Epstein Barr virus (EBV). Liver enzymes were trending up: alanine aminotransferase (ALT) from 153 U/L to 281 U/L, aspartate aminotransferase (AST) from 193 U/L to 685 U/L, alkaline phosphatase (ALP) from 143 U/L to 529 U/L, total bilirubin from 3.9 mg/dL to 9 mg/dL. Hemophagocytic lymphohistiocytosis (HLH) was highly suspected due to the clinical constellation of fever, splenomegaly, and laboratory results with marked cytopenias, low fibrinogen 158 mg/dL, significantly high LDH 1768 units/L, triglycerides 270 mg/dL, and ferritin 25383 ng/ml. Soluble interleukin 2 receptor (IL-2R) levels were obtained and were elevated at 31756.0 pg/mL (normal: 175.3-858.2 pg/mL). Bone marrow and liver biopsies were ordered, revealing the presence of hemophagocytosis [Figure 1] in both liver and bone marrow aspirates, diffuse Epstein-Barr Virus encoding region in situ hybridization (EBER-ISH) positivity [Figure 2A] in both liver and bone marrow core biopsies, and the presence of an associated clonal cytotoxic T-cell population satisfied the diagnostic criteria for HLH. The patient was treated with methylprednisone and Rituximab with clinical improvement and trending down liver enzymes and bilirubin. The patient was discharged on a tapering dose of prednisone. On outpatient follow-up, the patient’s symptoms resolved, and laboratory results normalized.
Discussion: HLH is a rare and life-threatening syndrome classified into primary and secondary forms. In HLH, the immune response is dysregulated, leading to excessive cytokine secretion, known as a “cytokine storm.” Primary HLH is due to a defect in the perforin pathway, while secondary HLH is associated with infections, autoimmune diseases, and cancer. Viral-induced HLH is a well-identified cause of secondary HLH, with EBV being the most common viral trigger. The diagnosis of HLH is challenging and involves various criteria. Severe liver injury is rare but can occur in HLH cases. Treatment includes dexamethasone and etoposide, with rituximab showing effectiveness in EBV-induced HLH. Chemotherapy and stem cell transplants are used for primary HLH cases.
Conclusions: HLH is a rare immune dysregulatory disorder with challenging diagnosis and treatment. Despite common liver involvement, patients rarely can present with acute liver injury or acute liver failure. Accordingly, further studies are needed to better understand liver involvement and optimize management.