Background: SARS-CoV-2, which has caused a global respiratory disease outbreak is also known to cause enteric infection and to present with gastrointestinal symptoms. Proton pump inhibitors (PPIs) are among the most commonly used medications in the U.S. and have been linked to possible adverse events such as an increased incidence of enteric infections and pneumonia. Early observational evidence suggests that PPI use may be associated with an increased risk of mechanical ventilation, admission to the intensive care unit (ICU), or death in patients with COVID-19. To date, an assessment of the relationship between use of a PPI during an inpatient hospitalization and clinically important disease outcomes has not been reported.
Methods: We used the MedStar COVID-19 Patient Registry to perform a retrospective, multicenter cohort study of consecutive patients hospitalized with COVID-19 in two urban academic medical centers in Washington, DC between March and April of 2020. Baseline characteristics consisted of demographics, pre-existing comorbidities, and initial laboratory values. All inpatient medications administered were also abstracted. Our independent variable was any inpatient administration of PPIs. Our primary outcome was mortality. Secondary outcomes included need for ICU admission. The Chi-Square test was used for all bivariate analyses involving categorical variables. Student T-test was used for bivariate analyses with normally distributed continuous dependent variables and Mann-Whitney U test were used for skewed continuous dependent variables. Logistic regression was used for multivariable analyses to adjust for all possible confounders, including age, race, comorbidities, and APACHE II score.
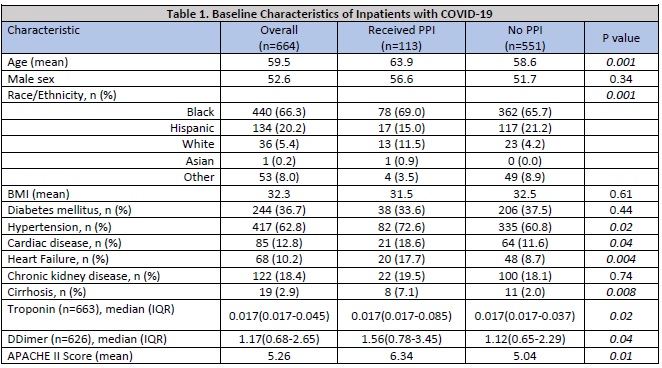
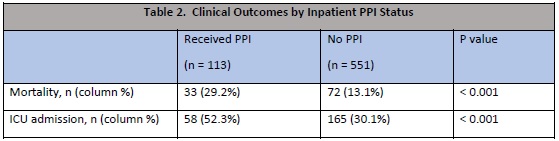
Results: We identified 664 consecutive admissions of patients hospitalized with COVID-19 from the MedStar COVID-19 Registry. Mean age was 59.5 and 52.6% of patients were male. Minority patients comprised 85.6% of the cohort (65.8% Black, 19.7% Hispanic, 5.5% White). Overall mortality rate was 15.8%. Older age, male sex, black race, several comorbidities, and APACHE II Score (on admission) were correlated with higher mortality rate. Inpatient PPI administration was reported in 113 (16.8%) of inpatients, and of these patients, 52 (46%) had a PPI on their home medication list. Compared with inpatients who did not receive a PPI, those who received a PPI were older, had higher rates of hypertension, cardiac disease, heart failure, and cirrhosis, and APACHE II score on admission (Table 1). In bivariate analysis, inpatient use of PPI was associated with increased mortality (29.2% vs. 13.1%, p < 0.001), and ICU admission (52.3% vs. 30.1%, p < 0.001). In multivariable analysis, inpatient PPI use remained independently associated with mortality (OR 2.03; p=0.05).
Conclusions: Inpatient PPI use was associated with increased mortality among patients hospitalized with COVID-19, even when controlling for age, comorbidities, and acuity at time of presentation in this multicenter cohort study. Clinicians need to be aware of the possible risks of this widely used medication and carefully assess the risk-benefit when deciding to administer PPIs to patients hospitalized with COVID-19. Further studies comparing outcomes stratified by indication for PPI prescription must be done to better characterize the risk associated with PPI use.