Background: Hip fracture (HP) involves bleeding that often requires blood transfusion and it can be life-threatening. Jehovah’s witnesses (JW) refuse blood products (BP) administration because of religious beliefs. Recombinant Human Erythropoietin (rHuEPO) has become an alternative but there are still no guidelines on its use in these situations.
Methods: JW patients with HP admitted to a level I trauma center between 01/JAN/2018 and 01/JUN/2023 were retrospectively evaluated. We analyzed demographic data, medical baseline conditions, type of injury, clinical complications, treatment and outcomes. Data are shown as percentage or median and interquartile ranges (quartile 1 – quartile 3)
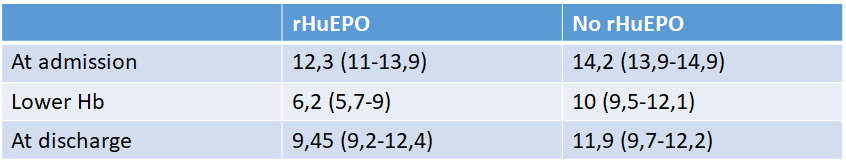
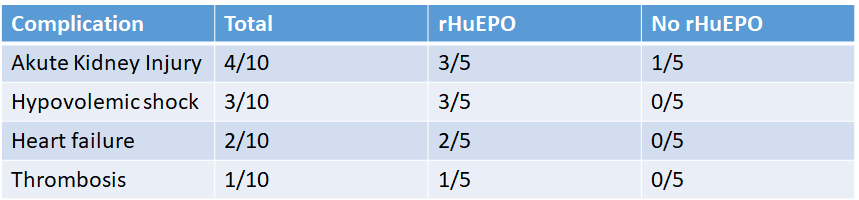
Results: Ten patients were included, 9 women. Median age at admission was 85 (79 – 86) years old. Charlson Comorbidity Index was 6.5 (5-8), 3 of them had history of atrial fibrillation (AF) and 1 an ongoing neoplasia. Polypharmacy was present in 7 patients, 3 were anticoagulated because of AF.The HP type was intracapsular in 2 of them, extracapsular in 7 and 1 periprosthetic hip fracture. At the time of admission the median hemoglobin (Hb) was 14.2 (13.8-15.1) g/dl, decreasing to 9.45 (6.2-10) g/dl after surgery. All patients received thromboprophylaxis with low molecular weight heparin and intravenous iron, none of them accepted BP transfusion. RHuEPO administration consisted of 20,000U subcutaneous (300UI/kg approximately). If multiple doses were needed, they were administred with a minimum gap of 2 days between them, guided by Hb levels. Five patients required rHuEPO, 4 with an extracapsular fracture and the one with the periprosthetic fracture. Three patients received a single dose after surgery and 2 required multiple doses, pre and postoperatively. Those who were treated with rHuEPO had a bigger decrease of Hb when compared to those without rHuEPO, 6.2 (5.7-9) g/dl vs.10 (9.5-12.1)g/dl. Median increased in Hb was a 18.7 (14-24)% up to a discharge Hb of 9.45 (9.2-12.4) g/dl in rHuEPO patients compared to 11.9 (9.7-12.2) g/dl in no-rHuEPO.During admission, the most frequent complications were acute kidney injury in 4 patients (3 in rHuEPO group vs 1 in no-rHuEPO), hypovolemic shock in 3 cases (all of them received rHuEPO) and heart failure in 2 of them (all in the rHuEPO group). One patient had a thrombotic complication which was superior mesenteric artery thrombosis. This patient had received 4 doses of rHuEPO and had a previous known atrial fibrillation that was not anticoagulated perioperatively.Length of hospital stay (LOS) was longer in rHuEPO patients, 25 (10-36.5) days, compared to no-rHuEPO group, 12 (10-43.5) days. Both groups seem to show a higher LOS compared to patients receiving BP. During the first year after HP 2 patients died, one during admission (10% of in-hospital mortality) due to the aforementioned thrombotic complication, another (non-rHuEPO) died after discharge due to an ulcer infection.
Conclusions: In our cohort, JW with HP suffered a similar mortality to previous reports but with a higher proportion of medical complications and a higher LOS. In the subset of patients requiring rHuEPO, the Hb decrease and these complications are specially severe. HP, mainly extracapsular and periprosthetic fractures, are at higher risk of bleeding and clinicians should start preventive measures after admission. RHuEPO may be an option in JW according to their comorbidities but more studies and clinical practice guidelines are needed to improve their management and determine the thrombotic risk.