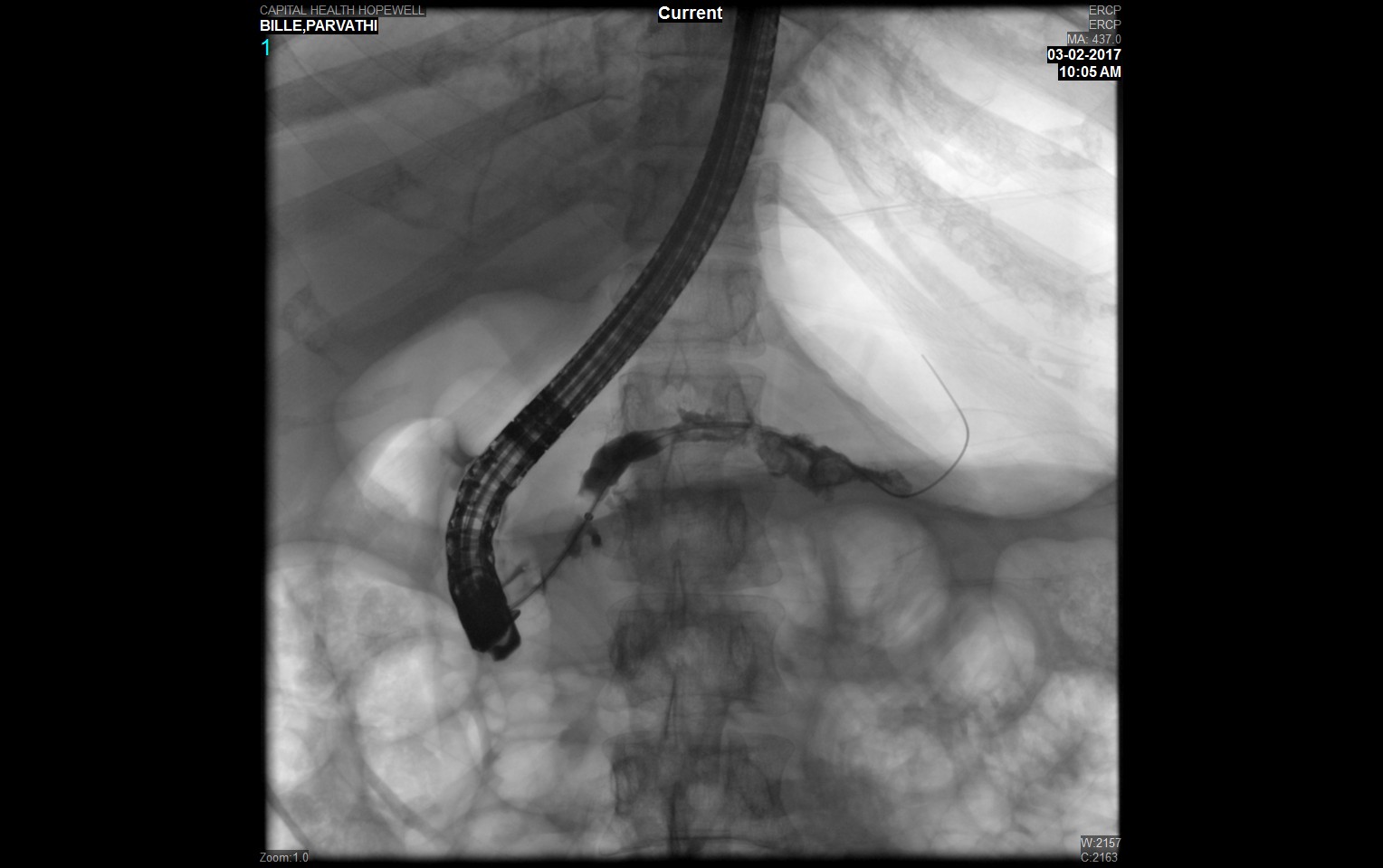
Case Presentation: This is a 35-year old Indian female, living in the United States for the past several years, presented with chronic mid-epigastric and left upper quadrant pain radiating to the back, nausea, and bilious vomiting. She complained of oily loose stools for the past 2 months. Her medical history is notable for insulin-dependent diabetes mellitus since 2008. She had her first episode of acute pancreatitis in 2005. During the past year, she underwent endoscopic ultrasound (EUS) once and ERCP three times. These investigations showed chronic pancreatitis complicated by pancreatic ductal stricture and pancreaticolithiasis. Endoscopic therapy was performed, including pancreatic sphincterotomy, balloon dilation, extraction of pancreatic duct stones, and stent placement. She denied alcohol, tobacco, or drug use. Her medications on admission were Insulin and Pancrealipase. There was mild tenderness of left upper quadrant and epigastric abdominal area without rebounding or guarding. Admission studies were notable for a glucose of 136 mg/dl, HbA1C 9.1%, LDL 114 mg/dl, HDL 30 mg/dl, TG 82 mg/dl, Hemoglobin 11.1 g/dl, and WBC 13.1 K/mcL. Abdominal CT noted acute pancreatitis with a 2.1 x 1 x 1 cm calculus in the pancreatic neck. Right upper quadrant ultrasound demonstrated a normal gallbladder and non-dilated extrahepatic bile duct. ERCP was done, a large calcified stone and frank pus were extracted and a pancreatic duct stent was inserted. She was given IV levofloxacin and the remainder of her hospital course was uneventful.
Discussion: Diagnosis of TCP is based on clinical history in the proper epidemiologic context, supported by imaging. TCP occurs most commonly in young adults and adolescents. It has become more heterogeneous as only a fraction of cases now fulfil the criteria of classical TCP. Many explanations have been proposed for TCP, including malnutrition, cassava consumption, familial and genetic factors, oxidant stress and trace element deficiencies. Of these, only genetic risk factors have been found to have associations, including alterations in the genes SPINK-1 and chymotrypsinogen C. These observations indicate that TCP is a complex multifactorial disease requiring extensive in-depth studies to better establish the role of individual factors in the pathophysiology of the disease.
Conclusions: Tropical chronic pancreatitis (TCP) is a juvenile form of chronic calcific non-alcoholic pancreatitis observed almost exclusively in patients living in developing countries in the tropical or near-tropical geographies. TCP classically presents as abdominal pain and steatorrhea with or without diabetes. When diabetes is present, TCP is often known as fibrocalculous pancreatic diabetes (FCPD). Compared to the average chronic pancreatitis patient, TCP patients are younger, have large intraductal calculi, have a more aggressive course of disease, and have increased risk of pancreatic cancer. When diabetes occurs within this context, it is usually of insulin-requiring severity but only rarely presents with ketosis.