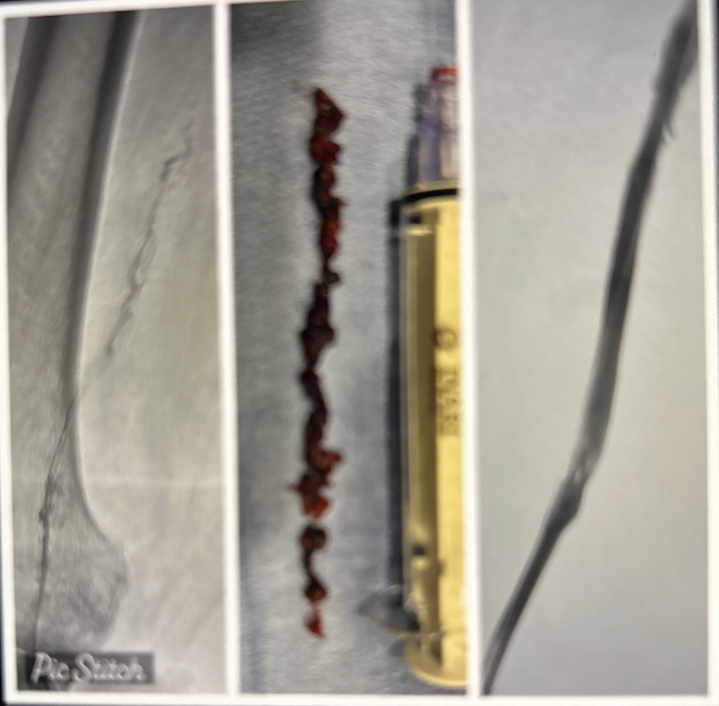
Case Presentation: A 61-year-old woman presented to the emergency department with a one day history of left leg pain. Of note past medical history is significant for coronary artery disease status post stent times two, coronary artery bypass graft (CABG), hypertension, hyperlipidemia, gastroesophageal reflux disease, heart failure with preserved ejection fraction, deep vein thrombosis (DVT) previously on Xarelto, and peripheral vascular disease status post right below-knee amputation in 2017. Patient noted severe pain from back of knee down to calf associated with numbness and tingling sensation while watching TV. She was sitting for approximately four hours. Persistence of pain led patient to seek medical attention. She had a 8.75 pack-year smoking history and is not an alcohol user. Patient’s family history is significant for a mother with recurrent thrombosis, especially of the lower extremities. On examination, the patient was hypertensive and hypoxic to 85%. She was started on 2 L nasal cannula. Her left calf was warm, swollen, and erythematous. A complete blood count was within normal limits. Basic metabolic profile revealed mild hyponatremia and elevated creatinine. Her prothrombin time was 12.0 seconds, activated prothromboplastin time was 30 seconds, and international normalized ratio was 1.0. CTA chest showed bilateral pulmonary embolism without heart strain involving few subsegmental branches of right lower lobe and left lower lobe pulmonary arteries. Venography demonstrated completely occlusive thrombus in the left distal superficial femoral vein and popliteal vein. Patient underwent left lower extremity thrombectomy and was placed on therapeutic Lovenox for one month. Interventional radiology was truly amazed at the size of the clot that was removed as it extended from the popliteal vein to the superficial femoral vein measuring as long as a 10 mL syringe, or 4 inches long. She was started on novel oral anticoagulation with Eliquis afterwards. Full hypercoagulability panel was unremarkable. She was appropriately discharged on Eliquis.
Discussion: This patient had a recurrent left lower extremity DVT for the second time that can not be explained by her chronic medical conditions, as none of them predispose her to a hypercoagulable state, except for morbid obesity. However, heart failure, smoking, and hypertension increase her risk of coagulation. She was also immobile watching TV for less than four hours duration. There is no set time of immobility that guarantees a DVT will form. All of her hematology/oncology work up so far to date has been negative. She does have a significant family history of DVT. Interestingly CTA chest showed bilateral pulmonary embolism, luckily for her only of the subsegmental branches and was hemodynamically stable on presentation. A second unprovoked DVT, has a high risk of recurrence and is usually treated indefinitely.
Conclusions: Patients who fail appropriate length of treatment for first unprovoked isolated distal (calf) DVT and present with another DVT should be treated indefinitely with anticoagulation as the risk of recurrence is high, as with our patient.