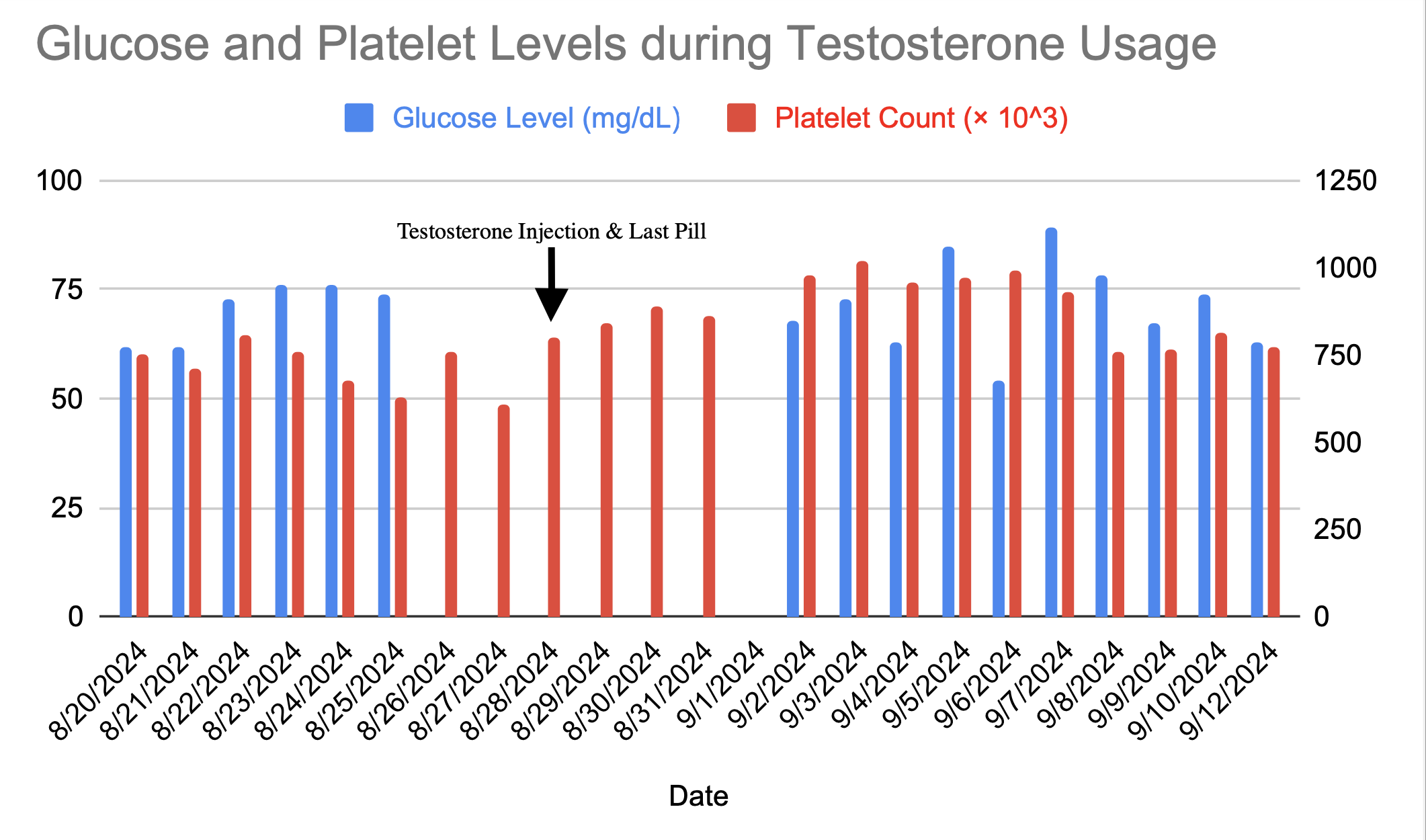
Case Presentation: A 44-year-old paraplegic male with chronic indwelling foley, chronic thoracic back pain, non-occlusive DVT, anemia, insomnia, and depression who presented with a three week history of abdominal pain, bilateral flank pain, chills, and fever was admitted for ESBL UTI. Hospital course was complicated by hypoglycemia and thrombocytosis due to exogenous testosterone use. During his hospital stay, blood tests repeatedly showed unexplainable hypoglycemia and thrombocytosis. Blood glucose levels were as low as 62 mg/dL, and platelet count ranged from 600,000 to >1,000,000/μL. All meals delivered to the patient were fully eaten, conveying no signs of a calorie deficit. Insulin, C-peptide, and cortisol levels were all within normal limits ruling out adrenal insufficiency or insulinoma. After several days of abnormal lab results, the patient disclosed using exogenous testosterone and supplements to improve his diminished leg strength from his paraplegia. Since admission, he took 3 testosterone supplement pills daily (300 mg) and 1 exogenous testosterone injection, ceasing after the study team was informed on day 9 leading to improvement in his lab values.
Discussion: Testosterone therapy and over-the-counter testosterone boosting supplements are subjects of ongoing debate, particularly regarding their safety and potential side effects. While testosterone therapy can benefit individuals with hypogonadism, it carries risks such as venous thromboembolism, sleep apnea, and weight gain. In this case study, we explore another risk of using exogenous testosterone and testosterone supplements: hypoglycemia. Testosterone therapy via oral, subcutaneous, or intramuscular administration routes has been shown to incite biochemical changes that induce increased insulin sensitivity [1]. Testosterone can increase lean muscle mass and decrease fat mass concurrently which can lead to decreased insulin resistance [2]. Many studies have shown this interaction with testosterone therapy within patients with type 2 diabetes (DM2). The risk of hypoglycemia for DM2 patients being administered both exogenous testosterone and insulin is now accepted as potentially harmful within the medical community [3]. The effects of manipulating exogenous testosterone use for DM2 are well-documented; however, research is limited when examining testosterone’s impact on patients who are not suffering from hypogonadism, pre-diabetes, or DM2. The number of testosterone therapy prescriptions is increasing annually due to its popularity and the rise in the number of men suffering from hypogonadism [4].
Conclusions: Research into the risk of hypoglycemia from exogenous testosterone in DM2 patients should potentially be extended to any patient considering hormone therapy, regardless of medical history. More research is needed to assess testosterone’s safety as its popularity grows.