Background: Keeping admitted patients in the emergency room (ER) carries negative operational and clinical consequences. Prolonged stays reduce ER bed turnover, thereby limiting access for other patients. Furthermore prolonged ER length of stay (LOS) has shown to be an independent risk factor for 30 day mortality for admitted patients. For these reasons, Veterans Affairs (VA) has set six hours as the goal for ER LOS for admitted patients. Lean improvement methods have proven useful in redesigning flow in many health care settings.
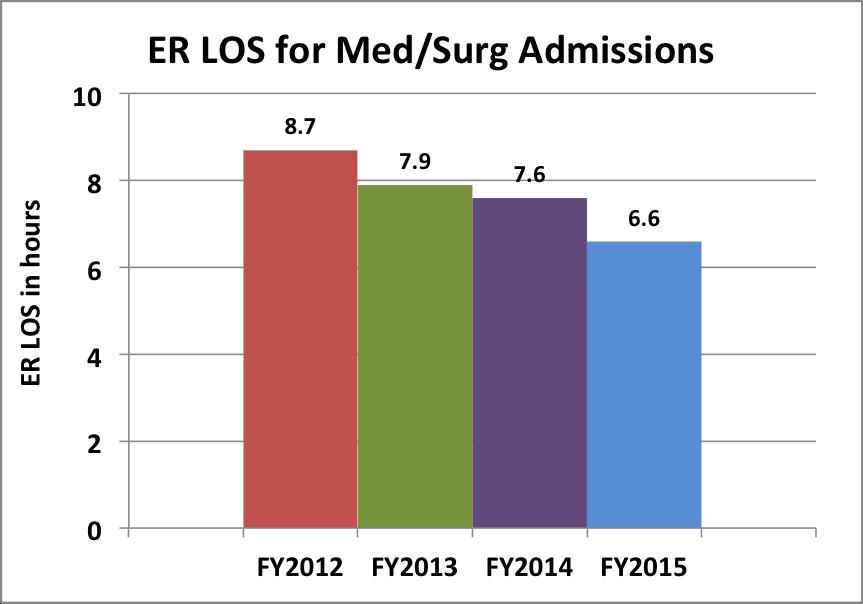
Purpose: At our institution, average ER LOS for medical and surgical admissions was 8.7 hours in 2012. We began a multidisciplinary process improvement project within a lean framework with the aim of reducing average ER LOS for medicine admissions to six hours or less.
Description: Our institution is an academically affiliated 90 med-surg bed hospital with approximately 20,000 ER visits and 5,000 medicine admissions per year. Through rapid process improvement workshops, root cause analysis identified three areas of focus: 1) inability to track time of initial consult to admitting team limited ability to evaluate delays 2) sequential evaluation by various members of the admitting team led to delays in admission orders needed for triage out of ER 3) lack of standardized hand-off between ER and ward nurses resulted in variable and delayed communication.
To address these root causes, this multidisciplinary team standardized the processes and time expectations for each of these three phases of an ER stay: 1) time stamps for admission evaluation requests 2) separating admission orders into part 1 (orders necessary to obtain the appropriate bed) and part 2 (everything else) and 3) creation of a standardized hand-off process from ER to ward nurses. As part of our institution’s overall lean transformation, the three key work units (ER, medicine physicians, ward nurses) developed a daily management system (DMS) which checked on the standard work that was created. Through DMS, we identified barriers to achieving the standard work and underwent multiple PDSA cycles to address them.
ER LOS for med-surg admissions pre-intervention in 2012 was 8.7 hours, and decreased to 6.6 hours in 2015 (Fig 1). We are currently comparing this difference in LOS to other similar VA facilities during the same time period for a difference-in-difference analysis.
Conclusions: Using a lean framework to identify root causes and develop countermeasures, we redesigned the admission process to significantly reduce ER LOS. While standard work was the foundation, monitoring the standard work through a daily management system and ongoing learning through PDSA cycles have led to sustained improvements.