Background:
Readmissions are a low‐value outcome for patients and costly to society. In the current environment there is ample motivation for hospitals and providers to improve this important patient outcome. Studies have demonstrated important reduction in readmissions through the use of 1 or more interventions. Nevertheless readmissions are complex problems without a single simple solution. In addition, some of the demonstrated interventions are cost prohibitive.
Purpose:
To reduce 30‐day readmission rate for general medicine patients cared for by hospitalists by at least 30% through the use of education, awareness, and a multidisciplinary team approach.
Description:
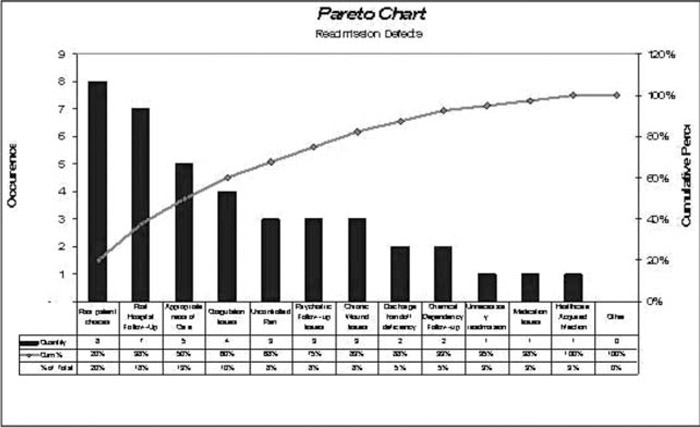
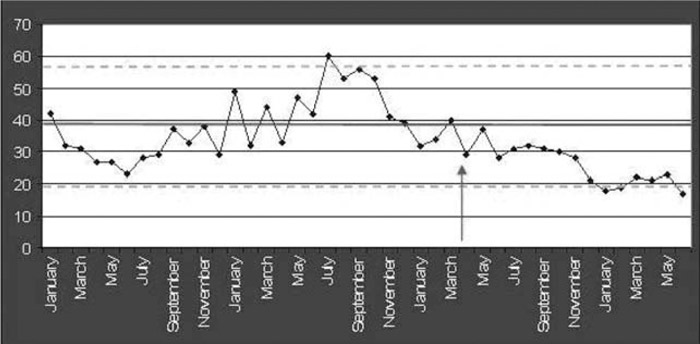
Our hospitalists formed a team composed of physicians, nurses, an administrator, and a physician assistant. Choosing a QI approach, we began by performing standardized reviews of our 30‐day readmissions. A Pareto chart of readmission causes confirmed the complexity and multiplicity of issues for our patients (Fig. 1), directing us to interventions that applied broadly to all patients, such as readmission awareness being raised by involving providers in formal reviews of their own readmissions and reflecting on potential preventability. Nursing staff initiated an early‐admission screen to identify patients with complex discharge needs that triggered early involvement by discharge planning. Communication with primary care providers was facilitated through a Web portal that allows them to view their patients’ medical records and by an invitation to discuss the case. Knowledge of risk factors for readmission and potential interventions was disseminated through pocket cards distributed to all staff. Discussion of the readmission risk was encouraged at daily bedside rounds to engage the patient/caregivers and at multidisciplinary rounds to encourage the full team to problem‐solve for the specific risk factors identified. Clinical assistants ensured all patients had timely follow‐up appointments, including INR checks within 4 days of discharge for those on warfarin. Readmission outcomes were discussed twice monthly at standing practice and division meetings. Outcomes were demonstrated using process control charts (Fig. 2), which were posted prominently and shared at meetings, by email, and on the divisional Web site.
Conclusions:
A multi‐faceted team approach utilizing education, awareness, and team engagement and using existing resources appears to be a viable approach to reducing 30‐day readmissions in general medicine patients on designated hospitalist units.
Disclosures:
D. Klocke ‐ none; A. Borrud ‐ none; D. Manning ‐ none; D. Kashiwagi ‐ none; K. Whitford ‐ none; D. Mann ‐ none; K. Hembre ‐ none; M. Burton ‐ none; D. Lawson ‐ none; N. Caine ‐ none