Background: Hospital readmission reduction has gained greater awareness since the passage of the Affordable Care Act and within it the Hospital Readmission Reduction Program (HRRP). Policy makers sought to improve quality of care by increasing reporting transparency and imposing financial penalties on facilities for excessive readmission rates. Baylor Scott & White Health (BSWH) remains committed to reducing hospital readmissions and in doing so improving the quality of care our patients receive in our integrated care model. In August of 2021, the Virtual Transitions (VT) program was created specifically to help address a system wide challenge and meet system wide goals related to readmissions.
Purpose: Patients are readmitted based on a variety of reasons from clinical progression to issues relating to social determinants of health. Through disruptive innovation, our team sought to create a patient-centered program to help navigate patients from the acute to the post-acute setting after an illness or flare of a chronic disease process. This journey of inter-professional collaboration utilizes telemedicine within an integrated health care system to improve quality of care and ultimately reduce hospital readmissions for those at an increased risk. After enrollment our patients are scheduled with one of our advanced practice providers who conduct a thorough assessment of not only clinical status but also social determinants of health that might ultimately contribute to a hospital readmission. Patients were eligible for the VT program if they had a readmission risk score of 16% or greater at any point during their admission, were discharged from a Hospitalist/Medicine physician and were discharging to home.
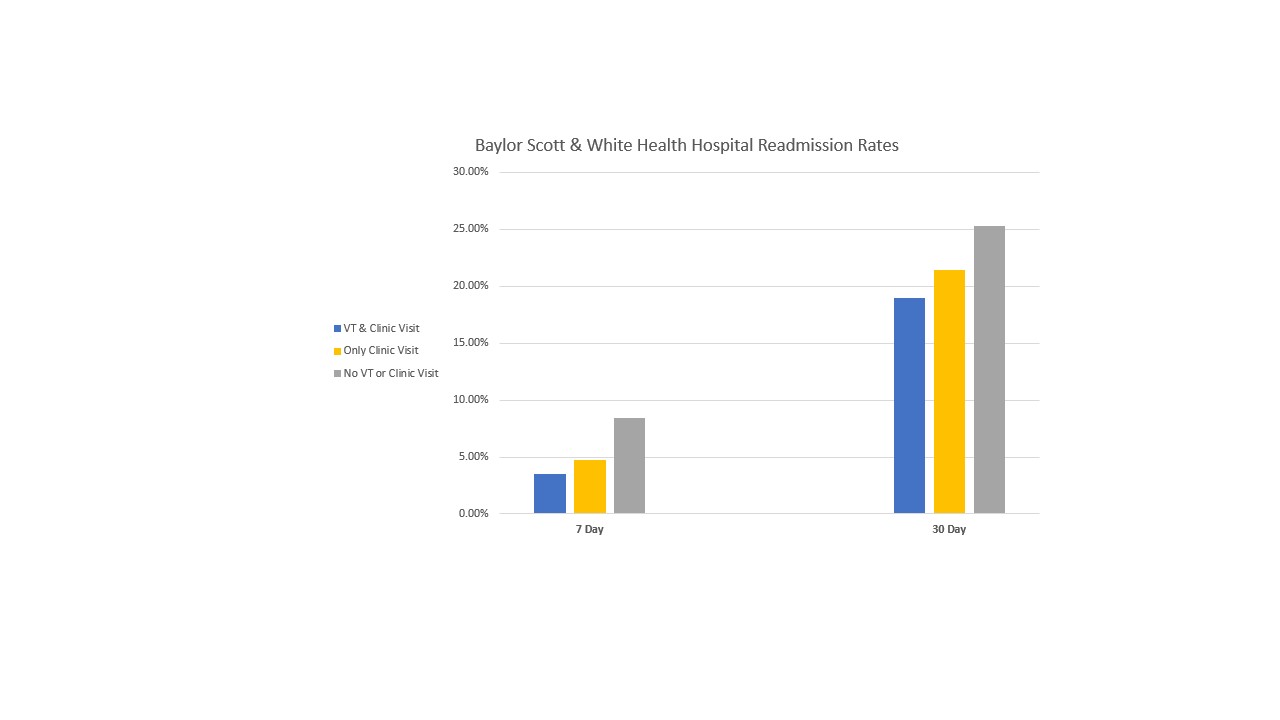
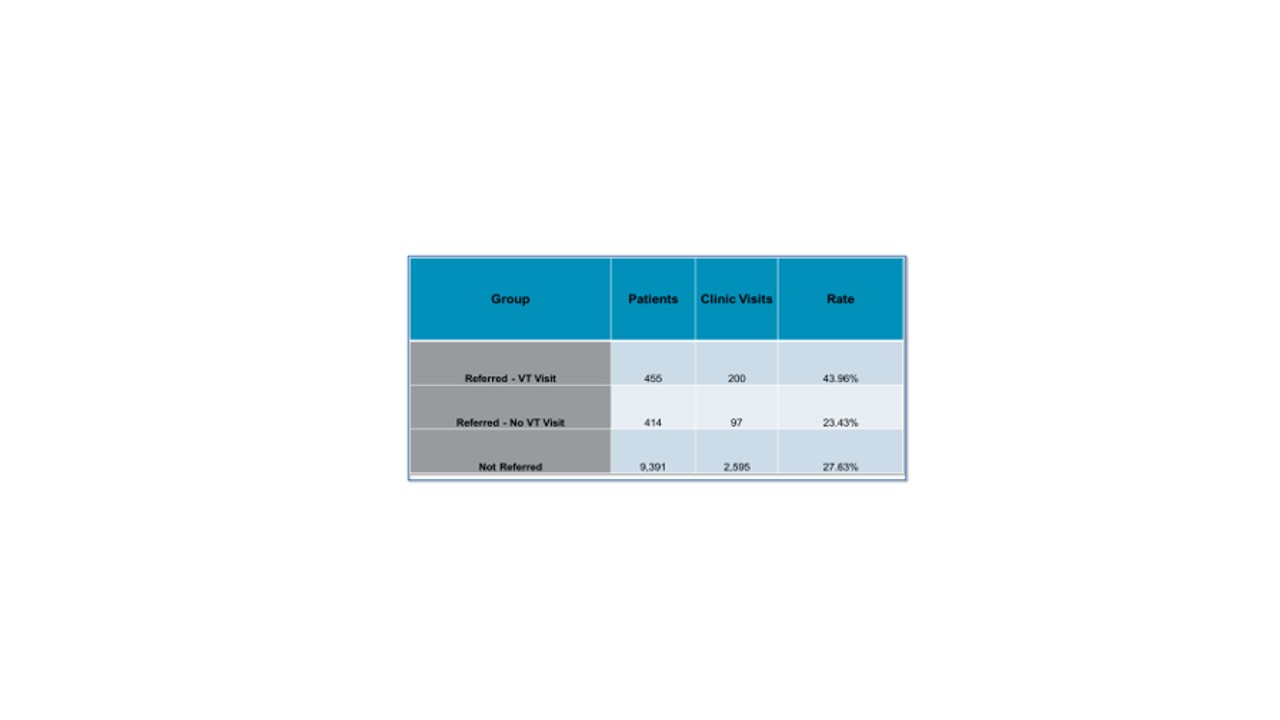
Description: Since inception in August 2021 through April 2022, of the 10,260 patients discharged from one of the six BSWH facilities affiliated with the VT program, 552 patients were successfully enrolled in our program. Our clinic saw 200 of those patients who also completed a standard in-clinic hospital discharge follow-up appointment – and of those only 7 (3.5%) and 38 (19%) were readmitted at 7 and 30 days, respectively. When compared to the control patient group of clinic visit without referral as well as the patients without any post-discharge follow-up, the reduction in readmission in the VT/clinic group represents a drastic improvement in hospital readmission reduction for those patients at an already increased risk of readmission. Additionally, patients who successfully completed a VT visit were almost twice as likely to complete their in-clinic hospital discharge follow-up.
Conclusions: Patients are readmitted to the hospital for a multitude of reasons and we aimed to develop a virtual clinic through a mindset of disruptive innovation to help navigate patients from the hospital bed and ultimately re-establish them with their PCP clinics. Our early data demonstrate that in patients with a readmission risk score of 16% or greater who are discharging from a Medicine team to home have a lower readmission rate when the standard in-clinic hospital discharge follow-up appointment is paired with at least one Virtual Transitions appointment. Furthermore, we have also shown a positive association with PCP clinic follow-up rate and provided a foundational recovery bridge from discharge to PCP clinics.