Background: Backup systems (jeopardy) are utilized by hospital medicine programs to staff clinical services in the cases of illness, leave and unexpected increases in clinical volumes. In the context of increasing hospitalist burnout and increased staffing needs during and after the COVID pandemic, a focus on how jeopardy contributes to clinician experience has emerged as an area of interest, but little is known about the structures of these programs and best approaches. We sought to characterize jeopardy systems and identify recommended practices for these programs across a broad sample of hospital medicine groups.
Methods: We conducted 5 semi-structured, virtual focus groups with a convenience sample of participants in the Hospital Medicine Reengineering (HOMERuN) Network to 1) describe the presence and structure of each jeopardy system and 2) discuss what is most fair, equitable and tolerable within these systems. Rapid qualitative methods using templated summaries and matrix analysis were then used to identify major themes and best approaches.
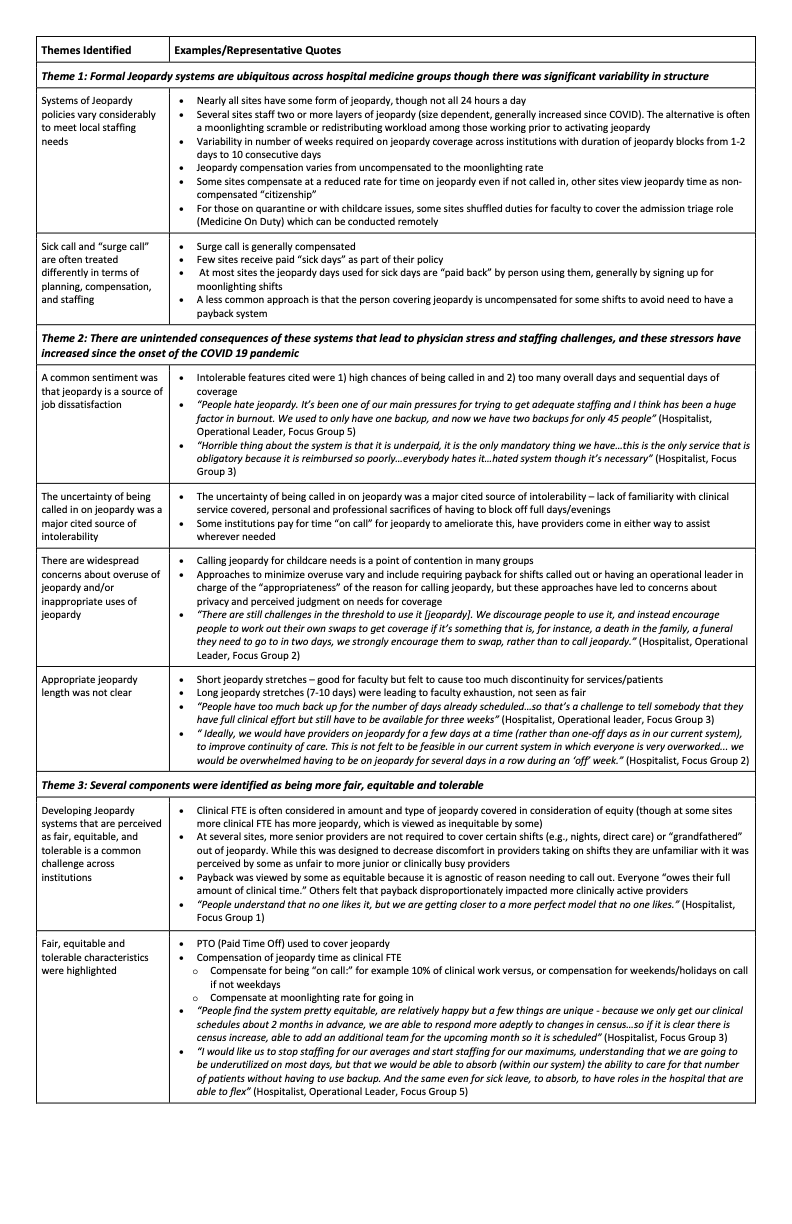
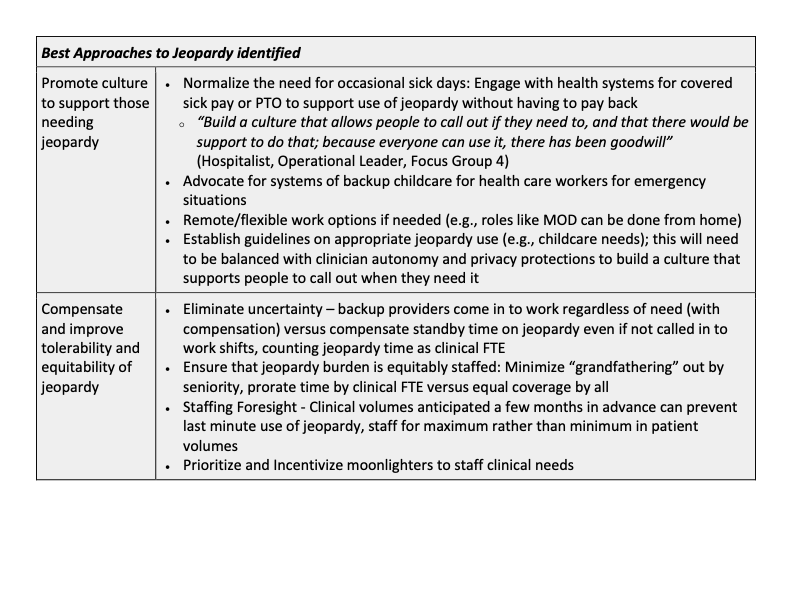
Results: Twenty-four participants representing 17 unique institutions (primarily academic) across 14 states participated in 5 concurrent focus groups. Twenty-two were hospitalist physicians and 8 were operational leaders in their institutions. Qualitative analysis revealed the following themes (Table 1): 1) Formal jeopardy systems are ubiquitous across hospital medicine groups, though there was significant variability in structure. The number of layers of jeopardy, amount of weeks of jeopardy per year, who covers it, and compensation for it varied widely. 2) There are unintended consequences of these systems that lead to clinician stress and staffing challenges, and these stressors have increased since the onset of the COVID 19 pandemic; 3) Several components were identified as being more fair, equitable and tolerable. Perceptions of best approaches to jeopardy structures identified included (Table 2): Normalizing the need for and providing coverage for occasional “sick leave”, maximizing built-in support structures for families, minimizing the uncertainty of the shifts, compensating for time spent on back-up, and distributing the jeopardy burden equitably across clinicians.
Conclusions: Jeopardy systems are common, but vary widely across hospital medicine groups. The majority of sites felt that, even though jeopardy programs are necessary, they are also a source of dissatisfaction that has worsened since the pandemic. Uncertainty of coverage, inadequate compensation and perceived unfairness in burden of coverage were key areas of discontent. This study highlights themes of jeopardy discontent that can provide hospital medicine leaders a roadmap to improve their jeopardy systems.