Background: Early recognition of clinically deteriorating patients and subsequent deployment of rapid response (RR) teams can result in “rescue” and avert irreversible patient harm or death. However, early detection of clinical deterioration may be impeded by communication barriers between patients and healthcare providers. In a previous study we published, adult hospitalized primary language Spanish (PLS) patients had significantly higher disease severity at the time of RR events and an 18.5% increase in length of stay (LOS) after RR events, as compared to primary language English patients at a tertiary academic medical center.
Purpose: We hypothesized that language barriers may cause delays in activation of RR systems and affect the provision of care. Reliance on more objective criteria to trigger RR events for hospitalized non-English speaking (NES) patients could mitigate the impact of subjective components of the patient assessment on the decision to mobilize necessary resources.Thus, we implemented a quality improvement project using objective criteria to trigger RR team consultation versus RR event activation with an interpreter for all adult NES patients hospitalized at our institution.
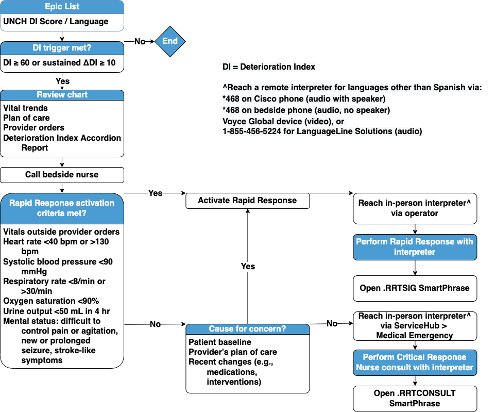
Description: Early warning scores (EWS) have been developed as alternative, more objective means for detecting clinical deterioration in hospitalized patients. Our hospital has adopted a proprietary Deterioration Index (DI) score that serves as an EWS; this is refreshed every 15 minutes and displayed in the EHR for all adult hospitalized patients. Our multidisciplinary team created a list in the EHR that populates with all adult non-ICU NES inpatients at our hospital. A column in the list displays each patient’s most recent DI score, the significance of contributing variables, and the change in score since last review. A workflow was developed directing the RR nurses to regularly monitor the list for real-time changes in DI scores and intervene based on pre-determined DI score thresholds (greater than or equal to 60 and/or a change greater than or equal to 10 since last review). All patient encounters are facilitated with interpreter services (either in-person or over-the-phone).
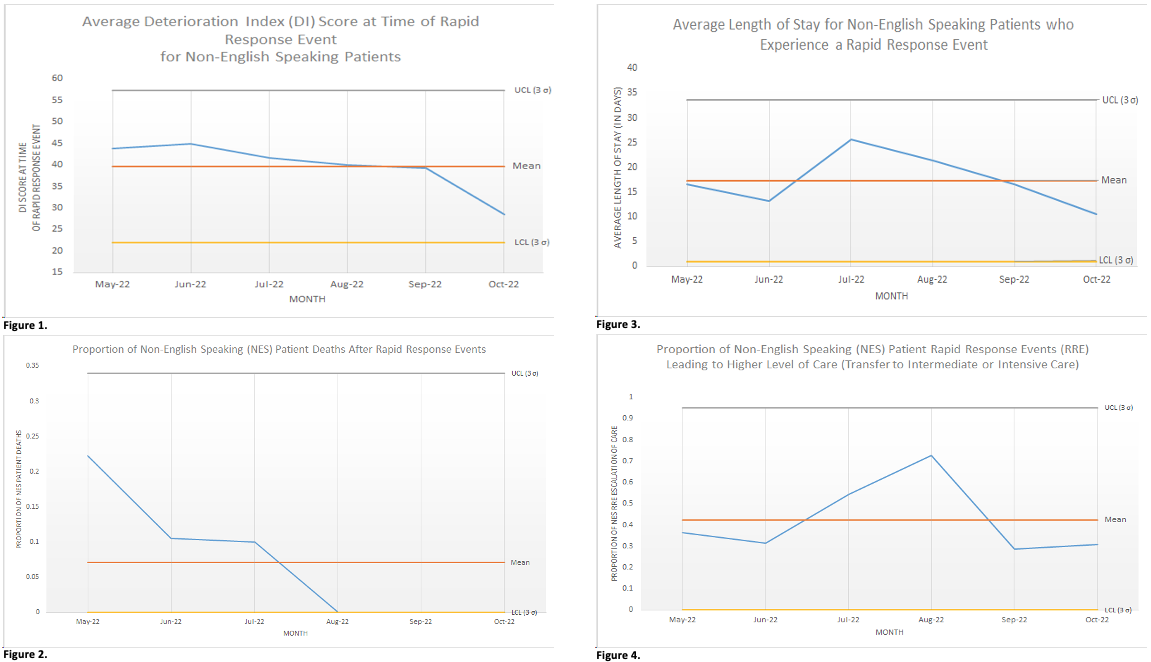
Conclusions: Preliminary project control chart analysis from 5/1/2022 through 10/31/2022 shows trends toward decreased disease severity at time of RRs and decreased mortality after RRs for NES inpatients (Figures 1 and 2, respectively). LOS and the proportion of NES patients requiring a higher level of care after RRs remain stable (Figures 3 and 4, respectively). Several unanticipated downstream affects have occurred since project start. First, we identified significant mischaracterization and incomplete reporting of preferred language, primary language, and interpreter need for adult inpatients at our institution and are now evaluating the effectiveness of the current process. Second, this initiative has introduced a new standard expectation that all RR events for NES patients utilize interpreter services. Qualitative feedback from stakeholders has been exceedingly positive and focused on the desire for accurate documentation of language preferences and interpreter needs, as well as the consistent utilization of interpreter services during RR events for NES inpatients.These findings support the hypothesis that consistent use of a system that circumvents the contribution of language as a barrier to the timely provision of essential medical resources can diminish gaps in equitable care delivery for NES hospitalized patients.