Background: In line with the American Board of Internal Medicine’s (ABIM) Choosing Wisely® initiative, the Society of Hospital Medicine (SHM) recommends not performing repetitive complete blood count (CBC) and chemistry (CHEM7) testing in the face of clinical and lab stability. In addition to decreasing the risk of hospital acquired anemia (HAA), reducing unnecessary routine blood work can ultimately result in significant cost savings for hospitals by directly decreasing laboratory costs and improving patient satisfaction.
Purpose: Our aim for this project was to determine if we could reduce routine laboratory testing frequency in the inpatient, teaching, hospitalist service by educating the house staff medical residents.
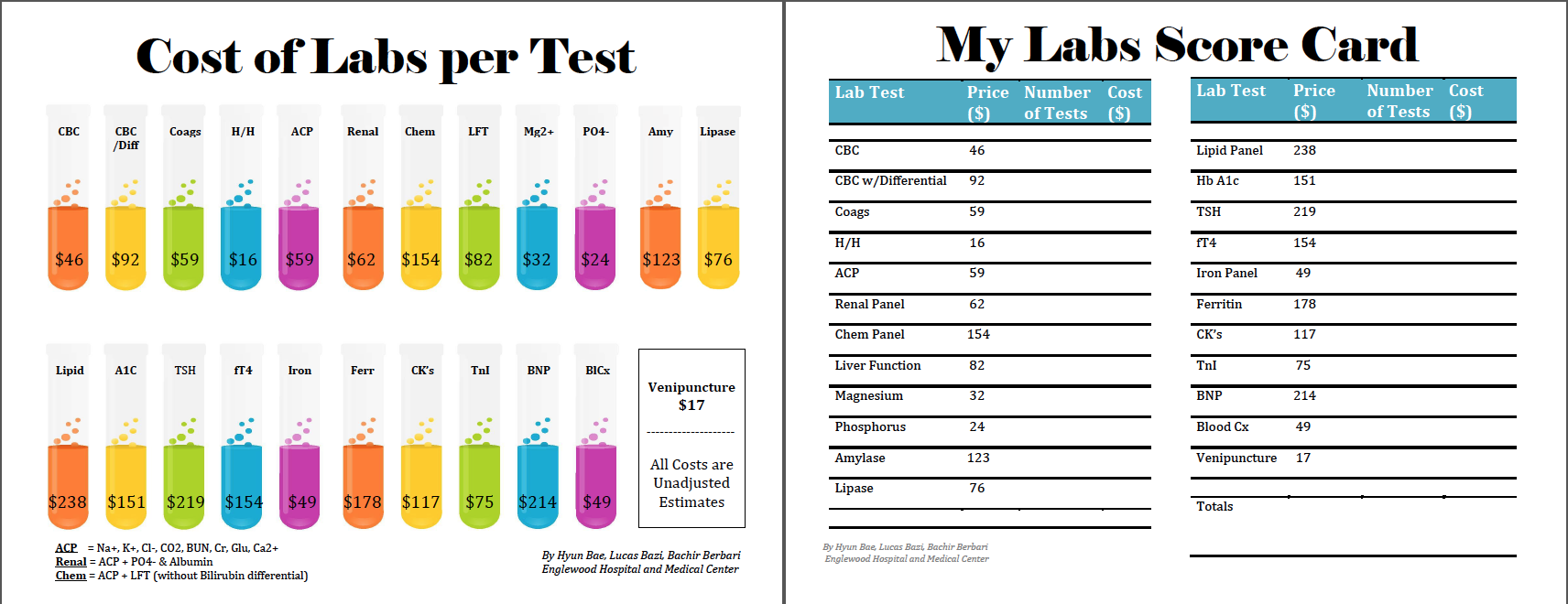
Description: We performed a prospective observational study in our community teaching hospital, comparing the number of common routine labs ordered per patient per day, before and after educating the medical residents working on non-ICU inpatient floors. We included all patients age ≥18, admitted under the teaching hospitalist service with a length of stay ≥12hrs, without any time in the ICU during that admission. Our interventions included monthly powerpoint presentations where residents were made aware of the cost of labs, asked to discuss the process of choosing labs to order, and practiced assigning indications for each lab ordered. We also distributed scorecards to aid the residents in monitoring their own performance. At baseline, our study population had an average of 2.42 common labs ordered/patient/day. After 12 weeks of intervention of educating residents, the outcome measure dropped to 2.36 common labs ordered/patient/day. Over the 12 weeks of intervention, the estimated amount saved was $17,875. Additional analysis of our data revealed that our highest outcome rates were in patients above the age of 64, and those with a diagnosis involving gastroenterology, cardiology or oncology.
Conclusions: An improvement in decreasing routine blood work was demonstrated through interval education of medical residents in an inpatient, teaching, hospitalist service. A reduction from 2.42 labs/patient/day to 2.36 labs/patient/day translated to an estimated cost saving of $17,875 over 12 weeks. Current interventions are being continued to see if our results are sustained. Further investigation is under way to see if additional interventions including hard stops on electronic orders of serial labs, and education of subspecialty consultants will improve our goals.