Background:
Blood cultures are frequently obtained by providers in the emergency department (ED) to evaluate pediatric patients presenting with fever. In pediatrics, nurses and laboratory personnel often obtain blood cultures at the time of placement of an intravenous catheter. Because of this collection technique, blood culture contaminants present myriad scenarios leading to unnecessary and costly interventions for the patient and the system. Published benchmark rates for contamination are 2%–3%. At our children's ED, we had a rate of 4% during the period from September 2008 through October 2009. The aim of our quality improvement project was to reduce the blood culture contamination rate by 50% in the children's emergency department by May 1, 2010.
Methods:
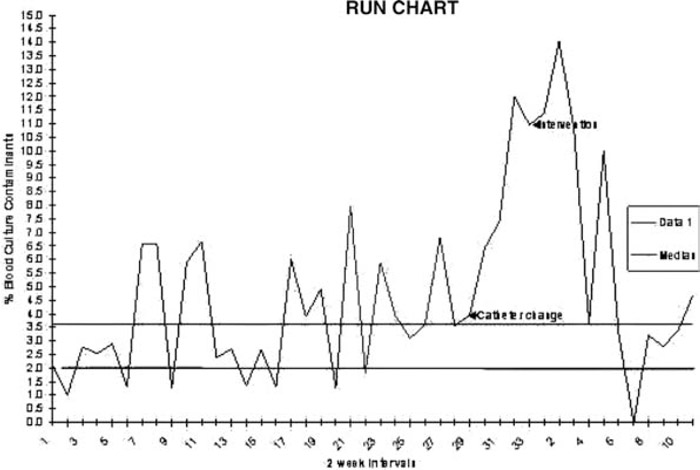
The number of contaminated blood cultures was expressed as a rate. Data were reported from the laboratory in 2‐week intervals following our interventions. Multidisciplinary brainstorming sessions were held to identify potential targets for intervention. Our initial intervention included standardizing the skin preparatory process, education regarding how to avoid contamination of the sterilized site, and proper preparation of blood culture bottle tops. A secondary intervention was also deployed as a blood culture bundle that included all necessary supplies as well as educational reminder cards/prompts to ensure the above primary intervention was followed.
Results:
A run chart was created to include the original, preintervention data (mean contamination rate, 4%), as well as our postintervention data (6.3% initially). These initial results were alarming and forced us to re examine unexpected trends and revisit our process analysis. We unveiled a change in process; specifically, a change in the intravenous (IV) catheter that was being used, which required a “2‐handed threading technique” versus “1‐handed technique.” This system change occurred in the 2‐month window between collected data points, prior to our interventions, and made the increase in contamination rate explainable (mean contamination rate with new catheter without intervention, 9.3%). We have since reinstated the original, preferred IV catheter and are now measuring the combined effects of both our interventions and improved equipment. Following both catheter change and interventional strategies, we did reach “0.”
Conclusions:
In the febrile, young child, obtaining blood cultures in the ED setting is a frequent practice. Standardizing technique and continued education can be used to reduce the contamination rate, yielding improved care and resource allocation. Unintended positive outcomes and observations can result from quality improvement measures.
Disclosures:
V. Hill ‐ none; M. Arandes ‐ none