Background: Chest radiographs (CXRs) aid in the evaluation of clinical status and assess the placement of new lines and tubes in patients in the Medical Intensive Care Unit (MICU). Despite studies documenting the safety of foregoing routine CXRs for stable, intubated patients and guidelines recommending against this practice, it remains standard in many ICUs.
Purpose: We aimed to change the culture of ordering routine CXRs in the MICU at our hospital with a goal to decrease total CXRs in the MICU by 30% over a 6-month period.
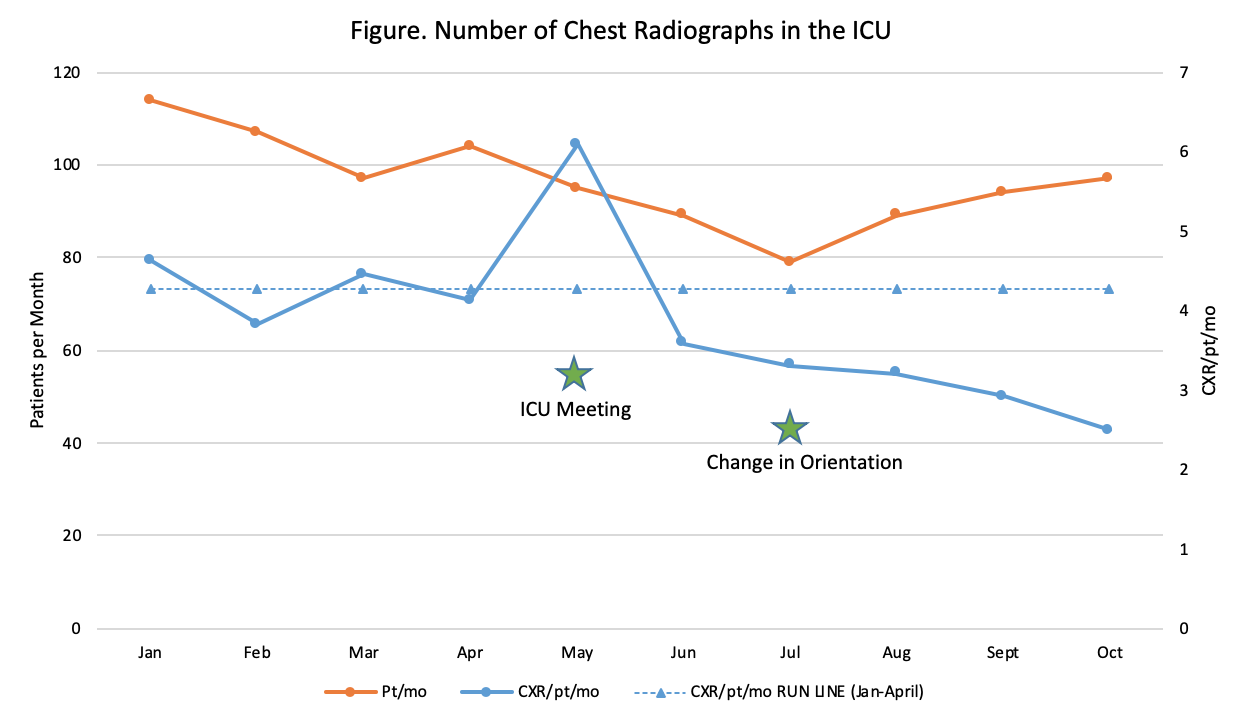
Description: We collected data from 1/18-4/18 for total number of CXRs, total number of patients, and average number of CXRs/patient/month (CXR/pt/mo) ordered in the MICU at our hospital to establish baseline trends. Using this data, we presented the project to the Critical Care team to gain stakeholder input and support for changing local practice (5/18). We then created laminated guidelines for each nursing station in the MICU and updated the resident orientation to include indications for ordering CXRs (7/18).Baseline data showed a mean of 4.26 CXR/pt/mo with 450 total CXRs/month. Over the last 3 months, following the formal change of orientation expectations, there are 2.98 CXR/pt/mo with 267 total CXRs/month (see Figure). This reflects a 30% decrease of total CXRs/month, adjusting for census changes.
Conclusions: With implementation of educational interventions and buy in from the MICU, we reduced the number of CXRs ordered in the MICU at our hospital. The charge of a CXR at our hospital is $180; resulting in average charges of $10,800/month. Decreasing the number of unnecessary CXRs also reduces radiation exposure to patients and decreases workload for radiologists and technicians.
Although our interventions have decreased the number of CXRs in our MICU, continued review of indications for ordering a CXR is important to continue this culture change. Changing ordering practices can initially cause anxiety, however, following national guidelines can support attitudes associated with change. It has been notable how quickly our interventions have made an impact on the ordering practices, indicating that sometimes change only requires a spark, particularly when (1) evidence supports that local practice differs from recommended care and (2) relevant stakeholders support the change. Hospitalists should be involved in guiding and supporting changes that improve the value of care being delivered, even in areas of the hospital where they may not practice directly. We plan ongoing data collection to ensure our trends were not markers of seasonal variation, though correction for census trends argues against this being a sole driver. Additionally, we plan to work with other ICUs in our hospital to change their routine ordering practices.