Background: Asymptomatic bacteriuria (ASB), or bacterial growth on urine culture without localizing urinary symptoms, is common in hospitalized patients.1,2 ASB is often misdiagnosed as urinary tract infection (UTI) and treated with antibiotics3 despite no improvement in mortality1 and multiple harms associated with antibiotic overuse.4,5 To reduce treatment of ASB, many hospitals set urinalysis parameters (e.g. white blood cells above a specified cutoff) that must be met before a urine culture can be obtained (i.e., “urinalysis with reflex to culture”). While this intervention may reduce urine cultures in some populations,6 other studies suggest that reflex urine testing may inadvertently increase treatment of ASB.7,8 We aim to (1) describe stewardship interventions targeting urine culture practices (including the prevalence of reflex urine testing) and (2) evaluate the effect of adding vs. removing reflex testing on ASB treatment over time. Our primary outcome was the National Quality Forum (NQF)-endorsed metric for evaluating ASB treatment in hospitalized patients: the percentage of patients with ASB treated with antibiotics out of all patients with treated bacteriuria.
Methods: Hospitals participating in an existing prospective cohort study, the Michigan Hospital Medicine Safety Consortium (HMS), between 12/1/2016 to 2/5/2020 were included in our study. In late 2019 all HMS hospitals were surveyed on their stewardship practices—including those related to urine culture and reflex culture practices.2 Guidelines from the Infectious Diseases Society of America4 and National Healthcare Safety Network9 were used to classify patients as having UTI or ASB based on symptoms documented in the medical record. We compared the percentage of patients with ASB treated with antibiotics out of all patients with treated bacteriuria before vs. after adding or removing reflex testing using logistic regression with random intercept at the hospital level.
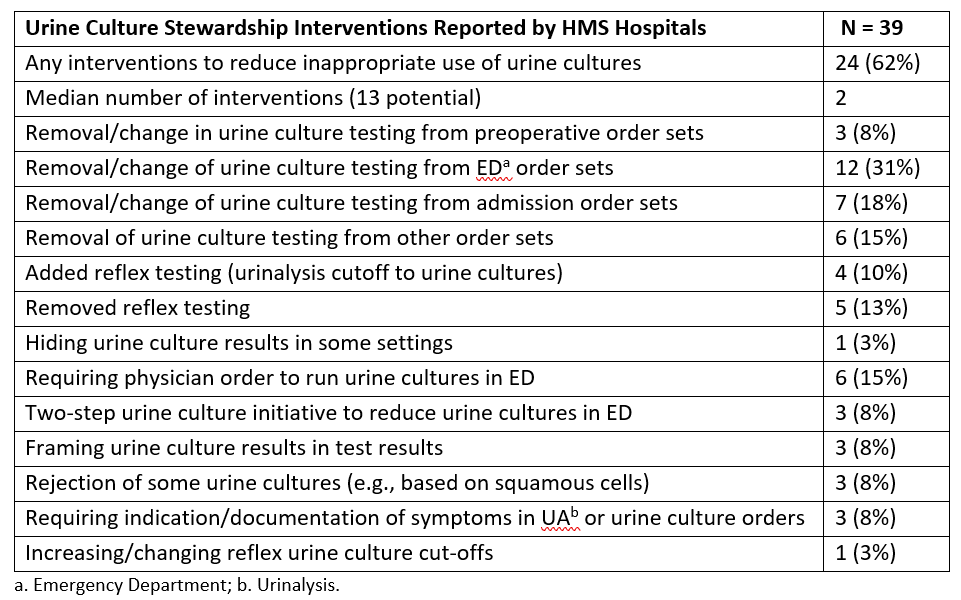
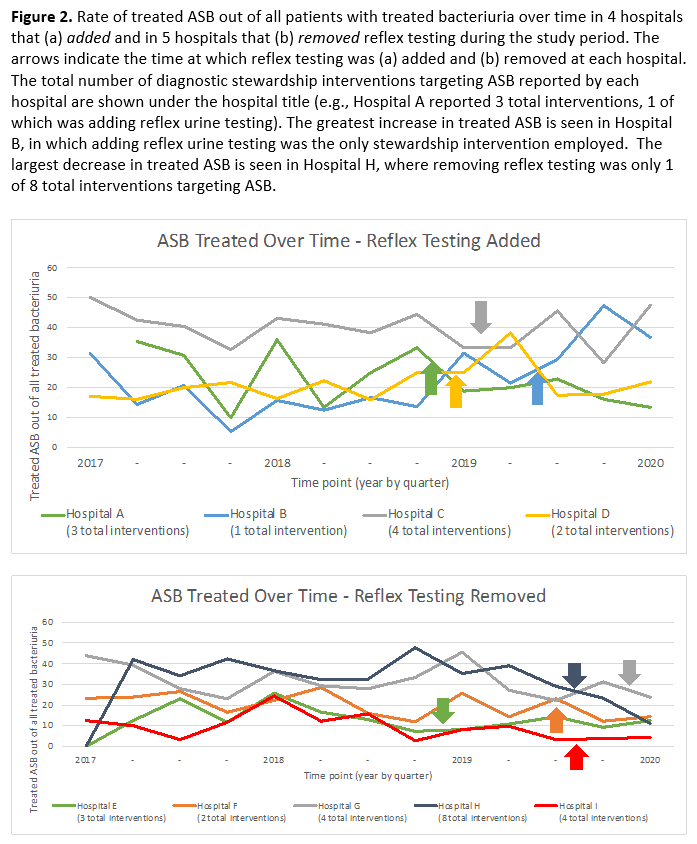
Results: Thirty-nine hospitals participated in the HMS Survey. Most hospitals reported implementing one or more diagnostic stewardship interventions targeting ASB (Table 1). Four hospitals (10%) reported adding reflex testing, while 5 hospitals (13%) removed reflex testing (Table 1); 20 hospitals (51%) reported always having and 10 hospitals (26%) reported never having reflex testing. Of 17,625 patients with positive urine culture, 15,804 (90%) were included of whom 30.5% (4819/15,804) had ASB. Of the 4819 patients that had ASB, 78.1% (3766) received antibiotic therapy for a median of 6 (IQR: 4-9) days. The percentage of patients with ASB treated with antibiotics out of all patients with treated bacteriuria was 25.5% (3766/14751). Hospitals that added reflex testing had no change in the percentage of patients treated for ASB out of all treated bacteriuria (27.9% to 30.1%, p=0.80) (Figure 2a); whereas the percentage of patients with treated ASB decreased (25.2% to 14.6%, p< 0.001) in hospitals that removed reflex testing (Figure 2b).
Conclusions: Most hospitals reported employing stewardship interventions to reduce the inappropriate use of urine cultures. Specifically related to reflex urinalysis, our data suggest adding reflex testing had no effect on the treatment of ASB, while removing reflex testing was associated with lower treatment of ASB. These data suggest further studies are needed to determine the effectiveness of reflex urine testing as a stewardship intervention.