Background: Advance care planning (ACP) informs future medical decision-making, particularly for hospitalized patients with older age or serious illness. The majority of end-of-life conversations are led by hospitalists in the inpatient setting. Despite the importance of ACP in end-of-life care, health disparities exist, with racial and ethnic minorities less likely to have advanced directives and living wills. We aimed to understand the impact of an intervention to improve ACP documentation for hospitalized patients on health disparities at our institution.
Methods: We launched an intervention in February 2019 to improve the rates of documented ACP conversations for hospitalized patients. Our intervention targeted hospitalists and trainees, encouraging documentation of ACP conversations (including cultural or spiritual values, hopes, fears, sources of strength, goals for ongoing medical care, and end-of-life care preferences) for all hospitalized patients aged >75 or with advanced illness as measured by ICD-10 codes. Using electronic medical record (EMR) reports, we obtained data for patients who met inclusion criteria between July 2018 and December 2020. ACP completion was analyzed by patient-reported race (White/Caucasian, Black/African-American [AA], Asian, or Other), ethnicity (Hispanic/Latino or non-Hispanic), and preferred language (English, Chinese, Russian, Spanish). We used interrupted time series analyses (ITSA) to measure the impact of the overall intervention and the differential impact by race, ethnicity, and language.
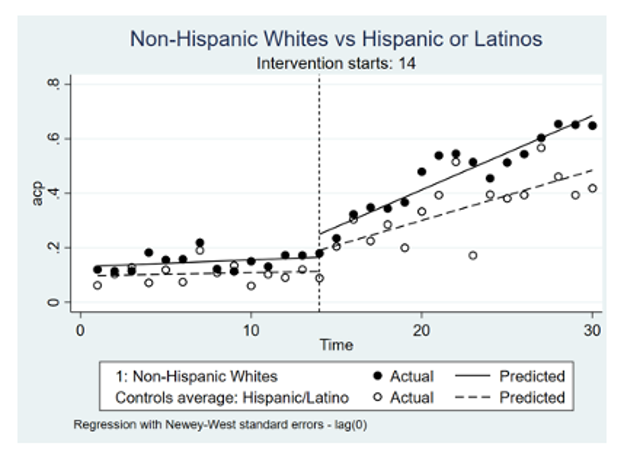
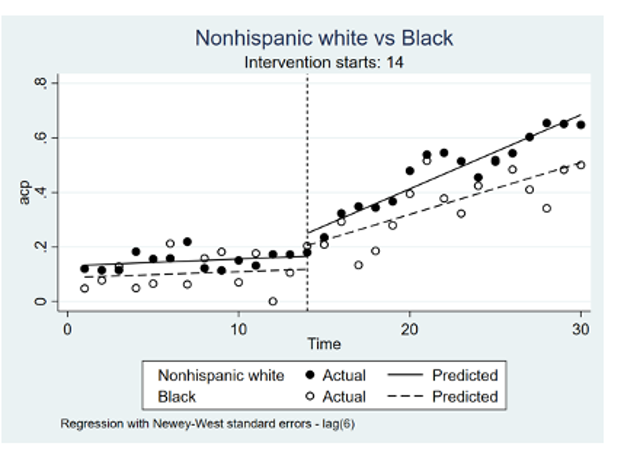
Results: 4,306 patients in the pre-intervention period and 5,914 patients in the post-intervention period met inclusion criteria. Using the year prior to the intervention as a baseline, January 2018-January 2019, overall rates of ACP documentation improved over 50% in the year following the intervention, with ITSA demonstrating a 2.47% increase in ACP documentation per month compared to baseline (p< 0.0001). During the post-intervention period the rate of ACP documentation increased by 2.72% per month for non-Hispanic white patients (p< 0.0001), by 1.84% per month for Hispanic/Latino patients (p< 0.0001) Figure (A); and by 1.9% per month for Black/AA patients (p< 0.0001) Figure (B). The difference between the post-intervention trends between non-Hispanic white patients and Hispanic/Latino patients and between non-Hispanic white patients and Black/AA patients were significant (p=0.0441 and p=0.0273 respectively). There were no disparities between English-speaking and non-English-speaking patients.
Conclusions: An intervention designed to improve ACP documentation resulted in overall improved rates of documented ACP conversations for hospitalized Medicine patients. However, the intervention had a differential impact on patients depending on race and ethnicity, with Hispanic/Latino patients and Black/AA patients seeing less of an improvement. Our finding of a disparity after a quality improvement implementation highlights the importance of measuring the impact of interventions on different patient populations.