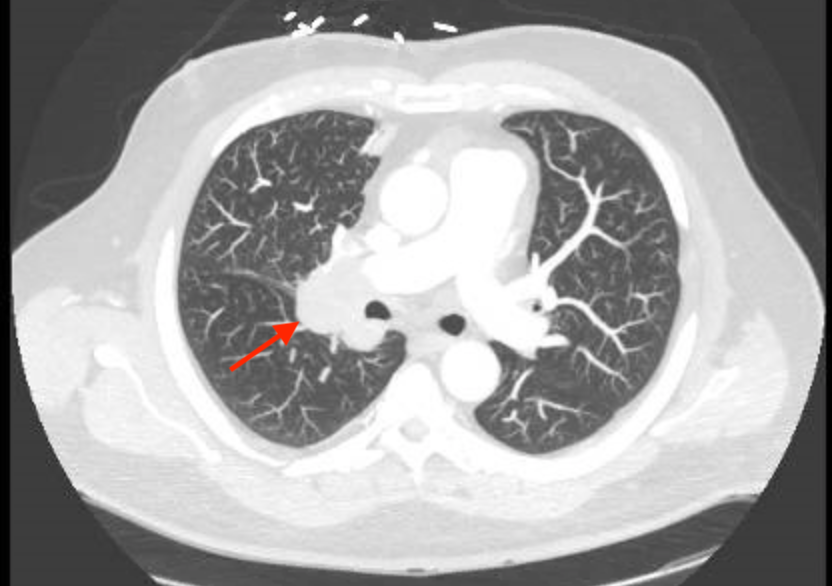
Case Presentation: A 55 year old Caucasian male presented to the emergency department with two weeks of palpitations and chest pain. He experienced intermittent chest pressure and palpitations that were worse while lying down. He denied recent change in weight, skin changes, or SOB. He had a 45 pack-year smoking history, having quit two years ago, with no other medical or surgical history. Serum chemistry was significant for a low serum potassium (2.5 mmol/L) and elevated bicarbonate (34 mmol/L), with sodium, chloride, creatinine, and troponin levels in normal range. LFTs showed an elevated AST (44 U/L) and ALT (168 U/L). Urine potassium was 29.6 mmol/L. CT imaging demonstrated a large right hilar mass with significant extrinsic compression of the right upper lobe bronchus and hepatic metastases. He was discharged on a high potassium diet and oral potassium supplementation. Liver biopsy was performed as an outpatient. However, his hypokalemia remained refractory to oral potassium supplementation and he returned to the emergency department four weeks later with severe hypokalemia and hyperglycemia. In that time interval, he continued to have palpitations and developed proximal muscle weakness, polydipsia, and polyuria. Liver biopsy results of his liver metastasis had returned at this time, demonstrating a poorly differentiated neuroendocrine carcinoma, consistent with small cell carcinoma. The patient was found to have a markedly elevated AM serum cortisol (70 ug/dL) and serum ACTH (153). Overnight low-dose dexamethasone suppression test demonstrated no reduction in serum cortisol. Aldosterone and renin levels were normal at 4.8 ng/dL and 8.2 pg/mL respectively. Results were consistent with an ACTH secreting small cell lung cancer. The patient was managed with IV and oral potassium, spironolactone, losartan, and ketoconazole. He received inpatient chemotherapy, his potassium eventually stabilized above 3, and he was discharged on oral potassium supplementation with outpatient follow-up for further chemotherapy.
Discussion: This case highlights a typical presentation of a rare clinical entity. The majority of lung neuroendocrine tumors are low-grade, well-differentiated and slow-growing tumors that rarely metastasize. This particular case represents a poorly differentiated, rapidly growing neuroendocrine small cell lung carcinoma with early distant metastases to liver and bone, with an initial presentation of refractory hypokalemia and hyperglycemia in the setting of ectopic ACTH production. The most common paraneoplastic syndromes associated with lung cancers are hypercalcemia and SIADH, followed by Cushing Syndrome. In this patient, the typical physical exam findings of Cushing’s Syndrome were not prominently present. Rather, the clinical symptoms associated with hypokalemia prompted the initial presentation and workup. Furthermore, this patient had no respiratory symptoms, increasing the importance of recognizing paraneoplastic etiology as a potential mechanism for his aberrant lab findings and initiating the appropriate diagnostic work-up.
Conclusions: In the absence of overt Cushingoid findings on physical exam, lab findings consistent with Cushing Syndrome should prompt consideration for ectopic secretion of ACTH, particularly of malignant etiology. In this particular case, the degree of ectopic ACTH secretion was correlated by the highly aggressive nature of the underlying neuroendocrine tumor.