Background: COVID-19 pandemic was vital in modifying healthcare delivery systems. This infection has led to variable composite outcomes in patients who have cardiovascular diseases [1,2]. In this study, we aimed to look into the impact of COVID-19 on incidence and outcomes of patients with Acute Myocardial Infarction using a nationally representative sample from the USA.
Methods: We analyzed national inpatient sample (NIS) discharge records for all admissions for AMI in the year 2020. Furthermore, we identified patients with and without co-morbid COVID-19 and assessed their demographic and co-morbid factors. Using propensity-matched cohorts, we estimated the impact of COVID-19 infection on the in-hospital outcomes of patients presenting with AMI. We assessed primary outcomes of hospital mortality and secondary outcomes of cardiac arrest, cardiogenic shock, respiratory failure, acute kidney injury, length of stay (LOS), and total hospitalization charges (THC) between both groups of patients.
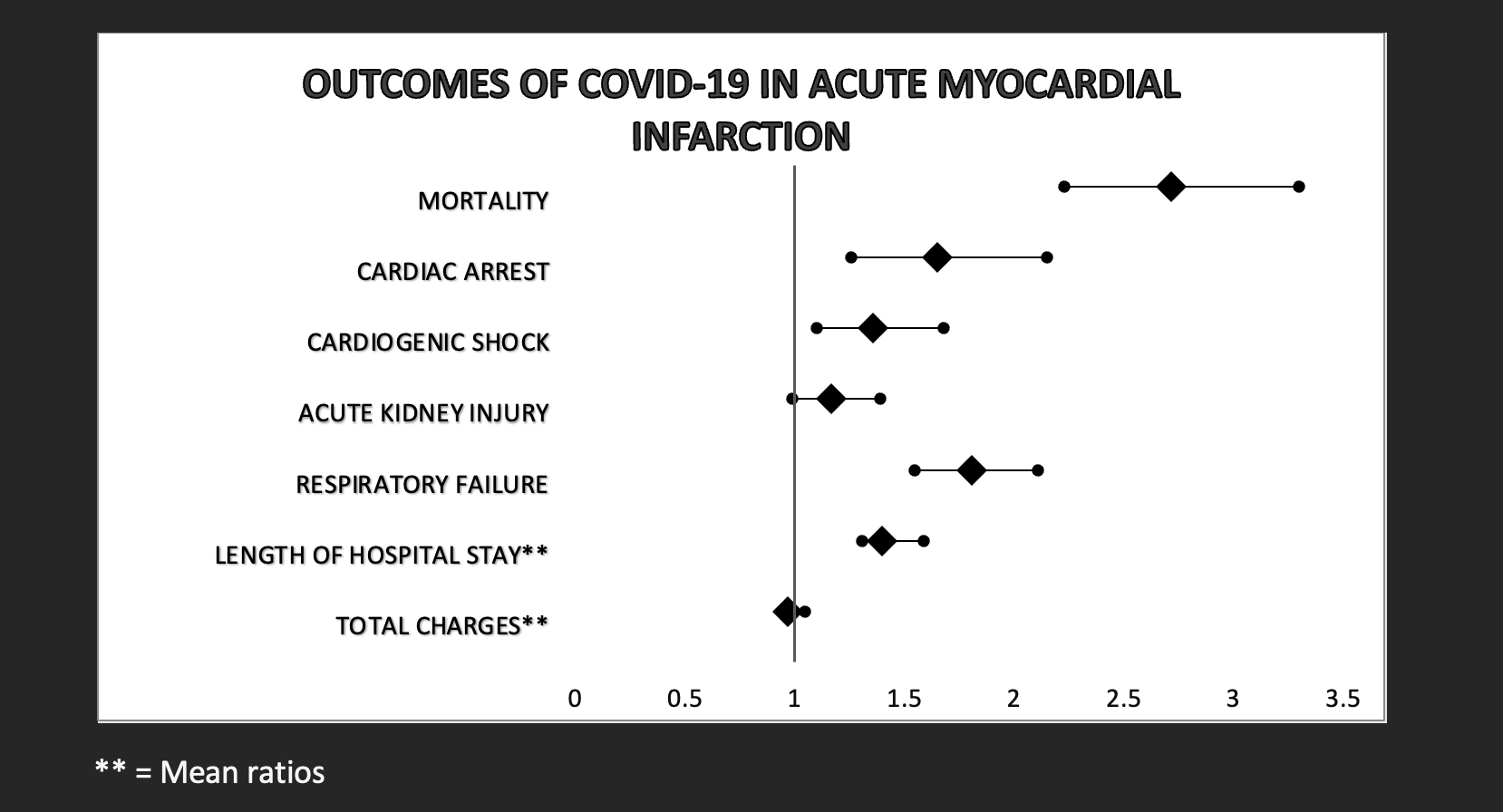
Results: There were 567,990 patients admitted for AMI during the study period. Following propensity scores matching, we identified 1,154 patients with concomitant COVID-19 infection who matched 109,990 patients without COVID -19. The proportion of AMI and COVID rates in male vs. female patients was (63.9 vs. 36.1 p = 0.9157). There was also no significant difference in age or comorbidity burden using Charlson comorbidity index. However, patients with COVID-19 and AMI were less likely to have traditional risk factors for AMI, including dyslipidemia (64.6 vs. 70.4, P < 0.001), Peripheral vascular disease (PVD) (2.4 vs. 3.8 p =0.0017), smoking (23.5 vs. 28.2 p< 0.0001) Hypertension (37.1 vs. 40.1 p = 0.0040) and Carotid artery disease (1.1 vs. 2.5 p = 0.0020). After propensity score matching, COVID-19 was associated with higher in-hospital mortality rates (Adjusted odds ratio (AOR: 2.72, CI: 2.23 - 3.30, p < 0.001). (AOR: 1.65, 95% CI: 1.26 - 2.15, p< 0.001), cardiogenic shock (AOR:1.36,95% CI: 1.10 – 1.68, p = 0.004) and respiratory failure (aOR:1.81, 95% CI: 1.55-2.11 p< 0.001) in patients with COVID-19 infection. There was also a significant increase in hospitalization (Adjusted mean differences:1.40, 95% CI: 1.31 -1.59 p < 0.0001) in the COVID-19 group.
Conclusions: Patients with COVID-19 and AMI have lower rate of underlying dyslipidemia, PVD, hypertension, smoking and carotid artery disease. COVID-19 presents with worse hospital outcomes in patients with AMI, with significant hospital mortality rates, cardiogenic shock, and cardiac arrest. Association between the lower likelihood of MI risk factors and worse composite outcomes in patients with both COVID-19 and AMI needs to be further studied. Higher level of disease suspicion and situational protocolised medicine is needed for patients with AMI complicated by COVID-19 for timely intervention may be essential to improve outcomes in this subgroup of patients.