Background: Since the implementation of the Hospital Readmission Reduction Program, 30-day readmissions have decreased across the U.S. regardless of hospital teaching intensity. The effect of financial penalties on long term readmission rates has not been studied. Teaching hospitals serve as leaders in medical education, research, innovation, and patient care. Therefore, we examined whether long-term readmission rates for heart failure (HF), acute myocardial infarction (AMI), and pneumonia differed between teaching versus non-teaching hospitals.
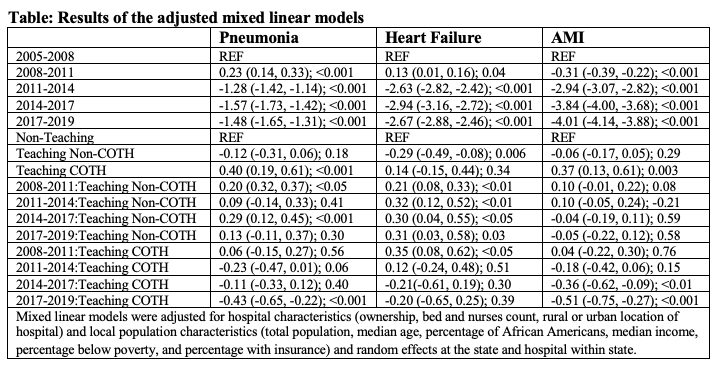
Methods: We used publicly available files from the Centers for Medicare and Medicaid Services (CMS) Hospital Compare program, which includes nationwide data on U.S. hospital characteristics. We defined teaching hospitals as those who receive graduate medical education funding from CMS. Teaching hospitals were further categorized into those who were members of the Council of Teaching Hospital and Health Systems (COTH) and those who were not. Using data from 2005-08 as a baseline, we examined readmission trends in three-year increments (with 2019 being the last year of reported data). We used mixed linear models to examine readmission trends through these periods, with adjustment for hospital characteristics (ownership, bed and nurses count, rural or urban location of hospital) and local population characteristics (total population, median age, percentage of African Americans, median income, percentage below poverty, and percentage with insurance) and random effects at the state and hospital within state.
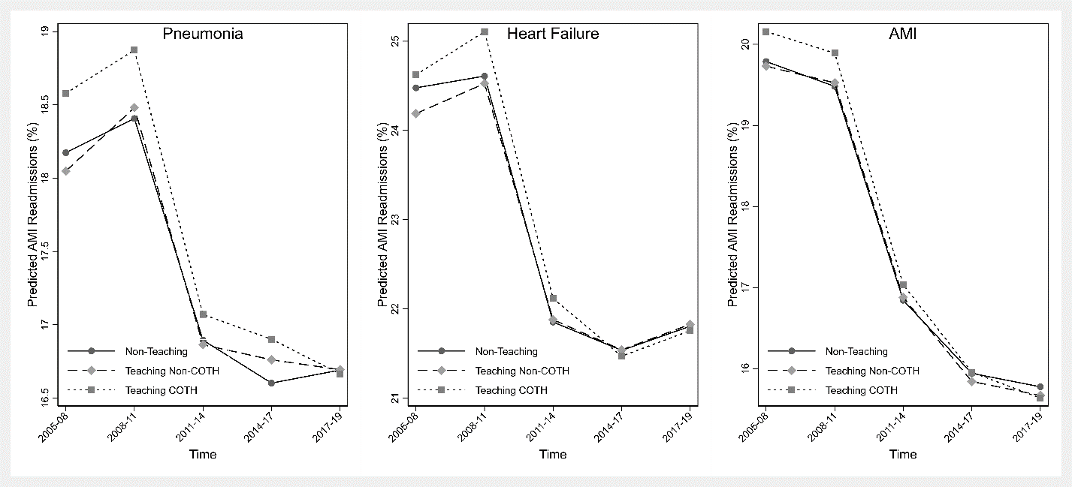
Results: Overall readmission rates for non-teaching hospitals were 18.2% (1.7), 24.6% (2.2), 19.8% (1.2), teaching non-COTH 18.2% (1.9), 24.4% (2.3), 19.9% (1.5), and teaching-COTH 19.0% (1.6), 24.9% (2.2), 20.4% (1.6) for pneumonia, HF, and AMI respectively. Of the 3310 unique U.S. hospitals, 2031 (61.4%) are non-teaching, 1061 (32.1%) are teaching non-COTH, and 218 (6.6%) are COTH-members. At baseline, there was no difference between non-teaching hospitals and non-COTH teaching hospitals for pneumonia, heart failure, and AMI readmissions. However, COTH teaching hospitals had significantly higher readmissions than non-teaching hospitals at baseline for pneumonia (0.59%; 95%CI = 0.37%, 0.81%) and AMI (0.43%; 95%CI=0.18%, 0.68%) but similar for heart failure. When comparing the baseline period with the most recent period (2017-19), COTH teaching hospitals had a significantly larger decrease in readmissions than non-teaching hospitals for pneumonia (-0.44%; 95%CI=-0.65%, -0.23%) and AMI (-0.51%; 95%CI = -0.76%, -0.27%). On the other hand, non-COTH teaching hospitals had a significant increase in heart failure readmissions than non-teaching hospitals (0.30%; 95%CI = 0.03%, 0.58%). These results did not change after adjusting for potential confounders except baseline heart failure readmissions (Figure & Table); teaching non-COTH hospitals had lower readmissions than non-teaching hospitals (-0.29%, -0.49%, -0.08%).
Conclusions: Our study findings show that despite higher readmissions at baseline in COTH teaching than non-teaching hospitals, readmission rates had a larger drop in COTH teaching hospitals during the observation period.