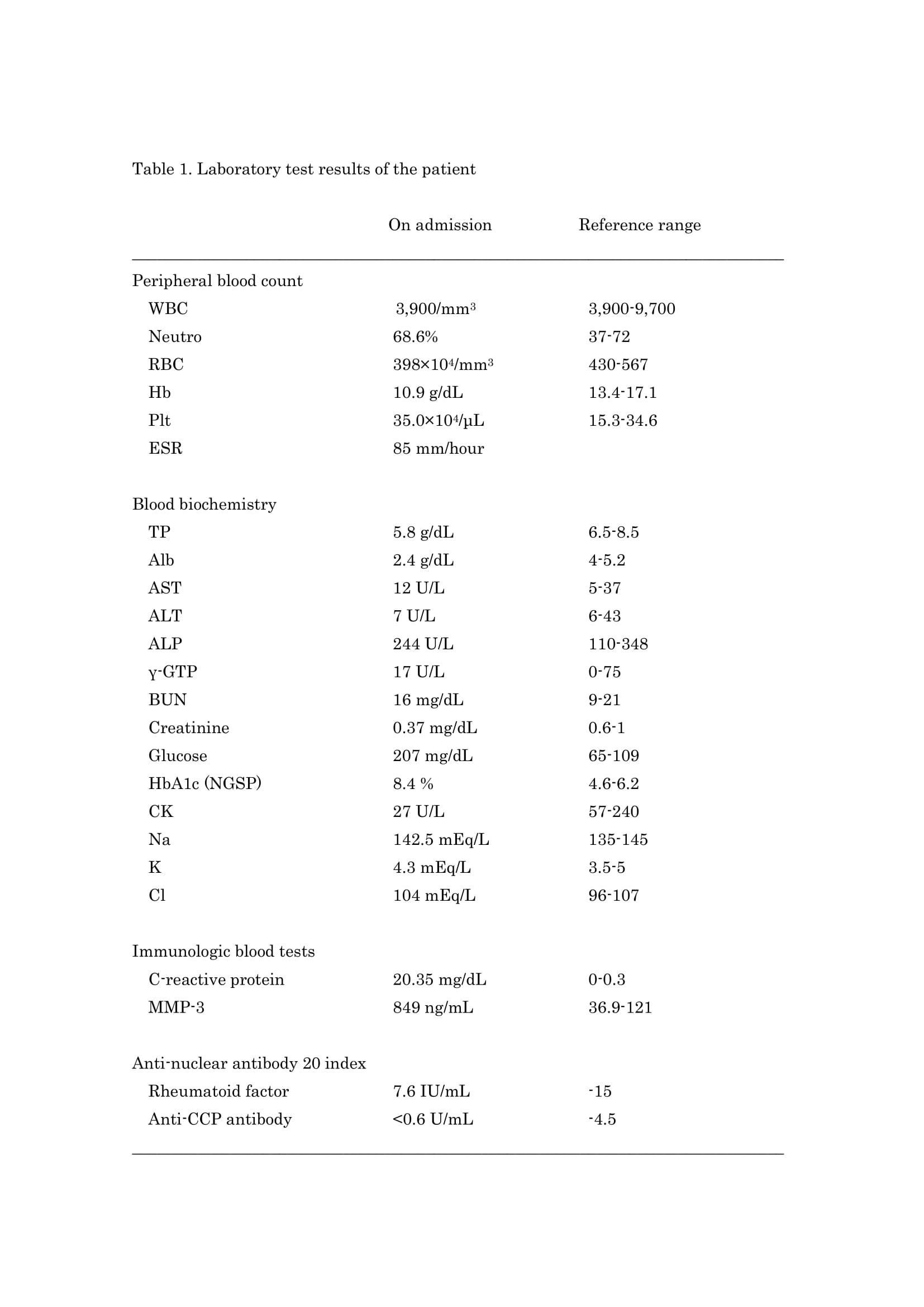
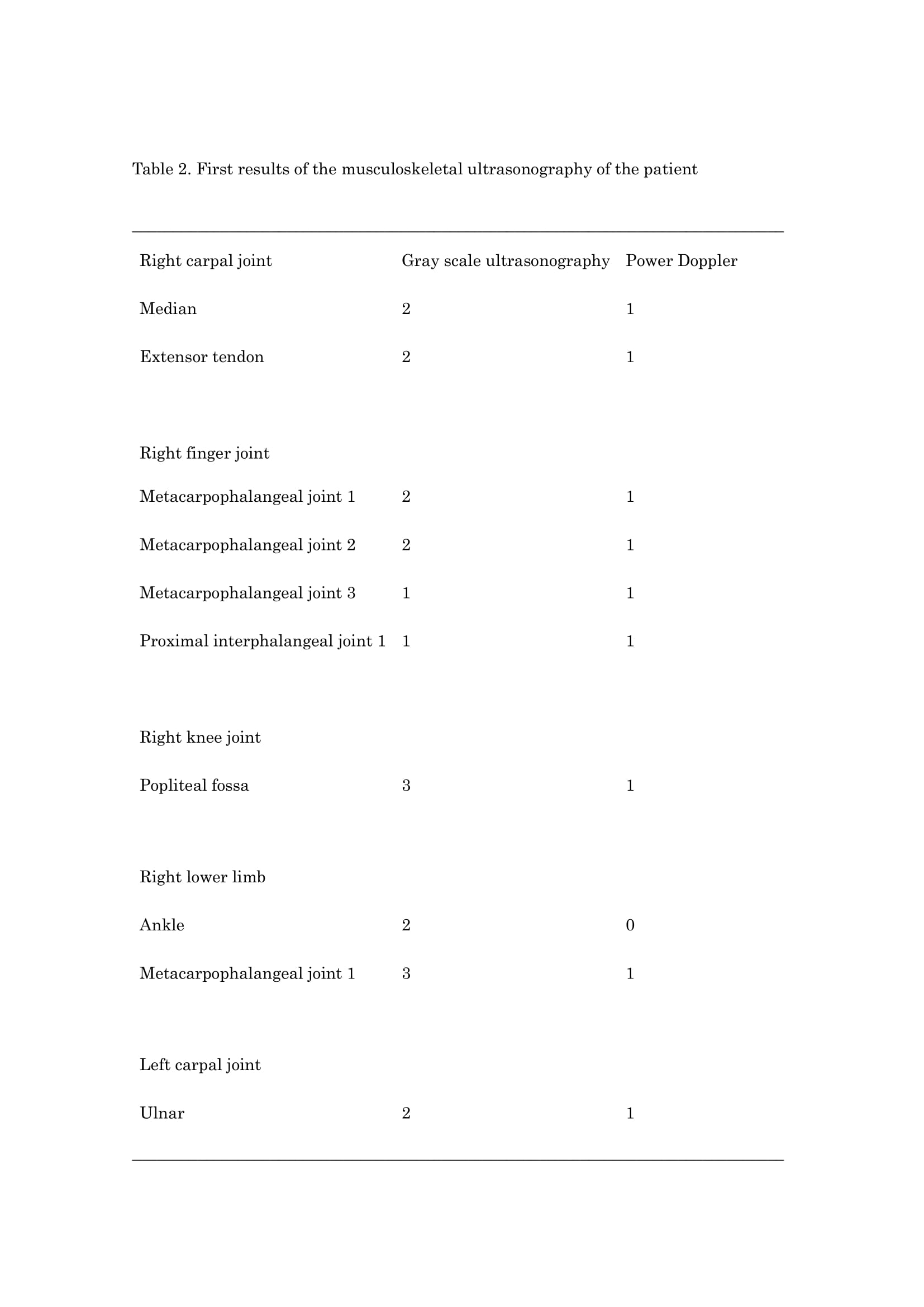
Case Presentation: A 73-year-old male patient was admitted to our hospital for fever, edema, and painful extremities. He has long-standing type 2 diabetes mellitus of 23 years. Four months before the present hospitalization, despite the body temperature of 37°C, he noticed edema, painful bilateral dorsum of the hands and feet, and poor physical condition. One month before this admission, he visited an orthopedic clinic and was prescribed antipyretic analgesics and diagnosed with pseudogout. His appetite gradually decreased, and he lost approximately 10 kg of body weight in 4 months. Because his symptoms did not improve, he visited a general hospital on the day before admission, and blood test results indicated severe inflammation, so he was referred to our hospital the next day. He had been taking the following medicines: two tablets of glimepiride 0.5 mg two times a day, three tablets of metformin 500 mg at three times a day, two tablets of vildagliptin 50 mg at two times a day, one tablet of empagliflozin 10 mg once a day, and three tablets of miglitol 25 mg three times a day. Upon admission, his general appearance and Glasgow Coma Scale were good. Physical examination findings were as follows: blood pressure, 137/61 mmHg; pulse, 101 beats/min; body temperature, 38.2°C; respiratory rate, 13 breaths/ min; and SpO2, 98% on ambient air. Examination of the distal portion of the extremities revealed slow-pitting edema. His pain level on the Numerical Rating Scale was 5/10; edema and pain were worse at the finger and carpal joints than at the interphalangeal joints of the feet. Blood test revealed elevated C-reactive protein, matrix metalloproteinase-3, serum glucose and HbA1c (National Glycohemoglobin Standardization Program) (Table 1). Among the cases we investigated, there were four reports of RS3PE syndrome due to vildagliptin. However, there was no clear report of other medications. From the above, the patient was diagnosed with RS3PE syndrome induced by vildagliptin, a DPP-4 inhibitor. We discontinued his glimepiride and metformin on admission. On the 6th hospital day, empagliflozin was discontinued. On the same day, musculoskeletal ultrasonography was performed, and peripheral synovitis and edema were observed in the lower limbs (Table 2) (1,2). On the 7th hospital day, vildagliptin was discontinued. His edema gradually improved from the 10th hospital day, and performance of activities of daily living also improved. On the 27th hospital day, musculoskeletal ultrasonography was performed again, and inflammation and edema disappeared completely. Thereafter, he recovered steadily. He was discharged on the 35th hospital day.
Discussion: RS3PE syndrome was first described by McCarty in 1985 (3). It is characterized by remitting, symmetrical, seronegative, rapid-onset synovitis, and pitting edema of the hands and feet. The present case satisfies the following diagnostic criteria for RS3PE acute bilateral symmetric polyarthritis: strong indentation edema on the back of bilateral hands, age≻ 50 years, and seronegativity (7-9). In recent years, RS3PE syndrome has been reported as a complication of diabetes (6,12) and as a side effect of DPP-4 inhibitors (13). In June 2015, RS3PE syndrome was added as a side effect to the package insert of DPP-4 inhibitors in Japan.
Conclusions: DPP-4 inhibitors are commonly administered to patients with type 2 diabetes. Since physicians frequently prescribe them, it is important to fully understand their side effects.