Background:
Thoracentesis is a commonly performed procedure to remove fluid from the pleural space. When repeat thoracenteses are required, patients are often referred to thoracic surgery to undergo more definitive treatment in the form of pleurodesis (talc) or Pleur‐X catheter placement. However, these procedures carry significant morbidity, and not all patients are well suited to tolerating them. Therefore, we analyzed a large series of thoracenteses performed at Cedars‐Sinai Medical Center to better understand the characteristics and outcomes of patients who opted for repeat thoracenteses.
Methods:
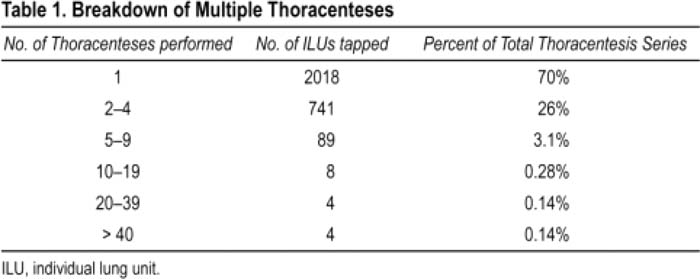
Data from a single proceduralist who performed 5000 consecutive thoracenteses over an 8½‐year period were retrospectively analyzed. Outcomes included the number of procedures performed per lung (tracked by individual lung unit, or ILU) and complication rates.
Results:
Four thousand eight hundred and ninety‐four thora‐centeses had complete data that could be analyzed. The overall complication rate was 2.3% (111 complications), with 29 (0.6%) classified as major. The procedures were performed on 2864 ILUs from 2207 patients (some patients had bilateral procedures). The number of procedures performed on each ILU ranged from 1 to 126 (Table 1). Of note, 7 “frequent flier” patients had at least 16 repeat thoracenteses, totaling 449 procedures, with 1 ILU undergoing 126 thoracenteses. Three of these 7 patients had liver failure, 2 had congestive heart failure, 1 had amyloidosis, and 1 had a history of lung cancer with a recurrent idiopathic effusion. An average of 50 thoracenteses per ILU was performed on these 7 patients, with an average removal of 1.7 L The complication rate for these 449 procedures was 1.1% (1 major = 0.2% and 4 minor = 0.9%); this was significantly lower than the rest of the series (P < 0.05). Of note, the idiopathic effusion patient went for pleurodesis (after 35 thoracenteses) and died postoperatively.
Conclusions:
Although the traditional approach to patients with recurrent pleural effusions is to refer them to thoracic surgery for definitive therapy, we identified a subset of patients who did well with repeat thoracenteses despite undergoing dozens of high‐volume procedures. Some of these patients were fearful of surgery, others were biding their time until transplant. Based on this analysis, we submit that managing patients with multiple thoracenteses is a reasonable treatment plan. Limitations to this study include that this was a retrospective analysis from a single operator, Further, patients may have had thoracenteses elsewhere with unknown complication rates. In addition, these data were collected at a tertiary‐care medical center with an aggressive thoracic surgery group. We did not track the number of our ILUs that eventually had surgical intervention, or their complication rates, Last, it is possible that in the absence of easy access to thoracic surgery, a larger number of our patients would have been managed with serial thoracenteses.
Author Disclosure:
M. Ault, none; B. Ault, none; B. Rosen, none.