Background: Warfarin and other anticoagulants increase the risk of hemorrhagic complications, including upper gastrointestinal hemorrhages (UGIB). Warfarin is commonly used in the management of atrial fibrillation to reduce the risk of ischemic stroke, and frequently resumed following UGIB. However, optimal timing of reinitiation remains unclear. Theory suggests that resuming warfarin immediately after UGIB would lead to additional hemorrhage and patient harm. Meanwhile, theory and cohort data suggest that delaying reinitiation contributes to increased risk of thromboembolism and increased mortality. Building on a previously-described microsimulation model of warfarin interruption, we set out to estimate the expected benefit of warfarin reinitiation as a function of day after UGIB, to identify the optimal day to resume warfarin following UGIB.
Methods: We extended a previously-described microsimulation model of patients with nonvalvular atrial fibrillation to incorporate the probability of rebleeding as a function of time following UGIB. Using that microsimulation model, we simulated identical cohorts of patients resuming warfarin at time points following UGIB to predict major events (ischemic stroke, intracranial hemorrhage, rebleeding, and extracranial major hemorrhages other than recurrent UGIB) and resultant morbidity and mortality. We simulated from a health system perspective over a lifelong time horizon, ultimately predicting discounted quality-adjusted life-years that would result from warfarin reinitiation on each day following UGIB.
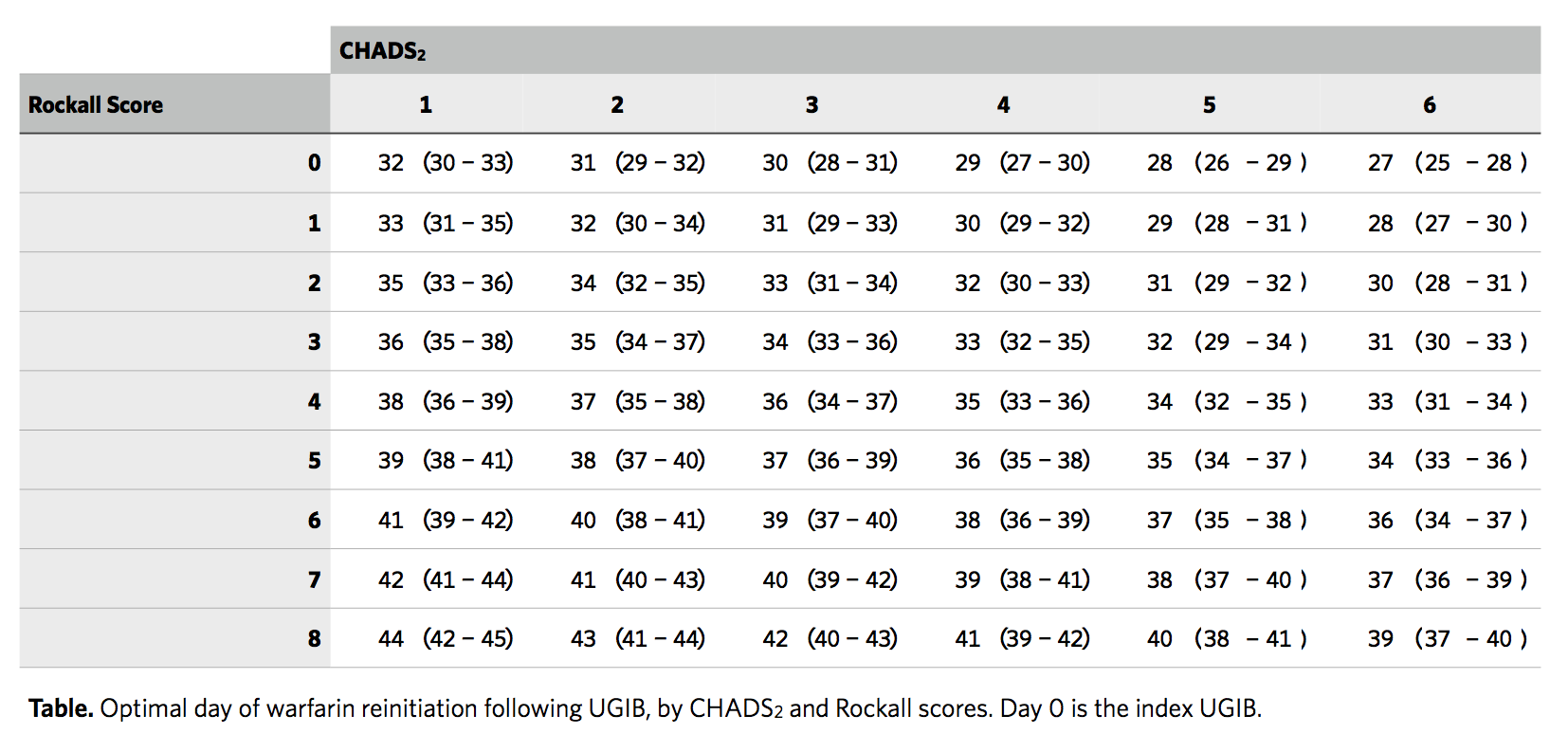
Results: In our base-case simulation of warfarin resumption following UGIB, reinitiation of warfarin 41 days following the index UGIB produced peak utility (see Figure). Resumption between days 38 and 44 produced greater than 99.99% of peak utility. In sensitivity analyses, optimal timing was later for patients who had higher probability of rebleeding (higher Rockall scores), and earlier for patients with higher probability of ischemic stroke (higher CHADS2 scores). Over the range of Rockall score, optimal day of reinitiation varied by around 12 days, while over the range of CHADS2, optimal day varied by around 5 days (see Table). Results were robust to a wide range of input parameters and conditions.
Conclusions: For unselected patients with nonvalvular atrial fibrillation managed with warfarin, our microsimulation analysis suggests that resumption around 41 days following UGIB is optimal for most patients. When discharging patients with nonvalvular atrial fibrillation following UGIB, hospitalists should request anticoagulation follow-up around that time. Time to reinitiation can be further personalized according to rebleeding and stroke risk, with rebleeding risk a more significant factor.
.png)