Background: Vascular access is an integral part of inpatient care. Difficult access can result in delays and inappropriate access selection or technical placement can have quality and financial implications, particularly those associated with catheter-line associated blood stream infections (CLABSI). At our institution, vascular access had historically been provider driven resulting in non-standardized selection practices with various teams of nurses, physicians, or contracted services fulfilling the requests, often in silos and with varying methods of documentation. We sought to improve the quality and appropriateness of vascular access by creating a multidisciplinary team to re-design the vascular access process. Our primary goal was to standardize indications, device selection, documentation, ‘difficult-stick’ protocols and provide complex access needs consultations. As a secondary outcome we predicted increased use of evidenced based central access and decreased use of contracted access services.
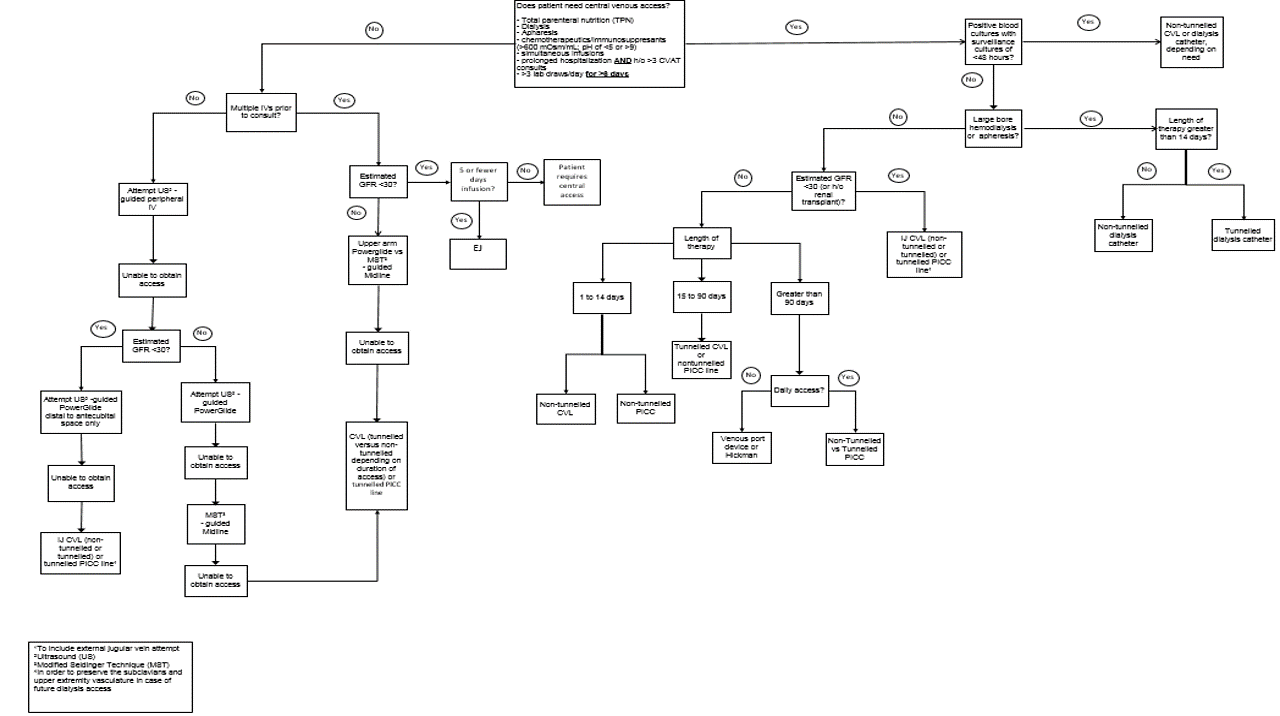
Purpose: In March 2017 we re-designed our processes to form a comprehensive vascular access team (CVAT) to provide consultation and procedures 24 hours daily. We re-engineered existing roles such as STAT IV and PICC RN positions to become CVAT RNs trained in access placement ranging from PIV to PICC and combined them with the physician run procedure service to perform CVL placements if necessary. Advanced Practice Practitioners (APPs) were hired to perform vascular access overnight. Using evidence based indications for line type, a vascular access algorithm was developed to guide device selection. An electronic consult order was developed to streamline the efficiency of consults, and a standardized documentation form developed. A training curriculum was developed and all CVAT RNs and APPs attended simulation based training on ultrasound guided vascular access including PIVs, midlines, and PICC lines. CVAT APPs attended an additional training session for central venous catheters. Each trainee then received at least 156 hours of supervised clinical experience performing vascular access procedures. This new comprehensive team used existing clinical coordinators to field consults and deploy the most appropriate resources based on clinical indications.
Description: Since inception CVAT has received over 4,300 consults with a median time from consult to procedure completion of 3.15 hours. PICC placement decreased from an average 240 PICCs per month in 2016 to 126 per month (March-October 2017) and contracted access services decreased from an average of 77 consults per month to zero, saving an average of $15,400 monthly.
Conclusions: Use of a comprehensive, multidisciplinary vascular access team can successfully reduce delays in vascular access. Additionally, the creation of this standardized evidenced-based approach to device selection likely reduced inappropriate central access.