Background:
Self‐mutilation has been defined as the deliberate commission of recurrent socially unacceptable direct physical harm to one's own body without conscious suicidal motivation. There is evidence that self‐mutilation has become more prevalent in the recent years. Self‐mutilating patients are often hospitalized for further evaluation and management and evoke strong emotional responses from health care providers. The goal of our descriptive study was to assess the prevalence and trends of self‐mutilation admissions at Saint Joseph Mercy Health System's (SJMHS) Ann Arbor, Saline, and Livingston hospitals over the past 9 years and to understand the demographic and clinical characteristics and cost burden associated with these patients.
Methods:
This was a retrospective observational study of patients hospitalized with self‐mutilation injuries at SJMHS from January 2001 to December 2008. Self‐mutilation cases included all patients discharged from SJMHS with an intentional self‐inflicted injury ICD‐9 code E 956.0–E959.9. The SJMHS Quality Institute database was used to obtain demographic information, information on comorbidities, length of stay, readmission rate, and mortality and to estimate the cost burden. Demographic, clinical, and outcome variables were summarized using means, medians, and percentages, as appropriate. We tested for increase in the overall admissions for self‐mutilation and the proportion of self‐mutilation of all self‐inflicted injuries using Cochrane‐Armitage tests of trend. We tested for cost trends using general linear models.
Results:
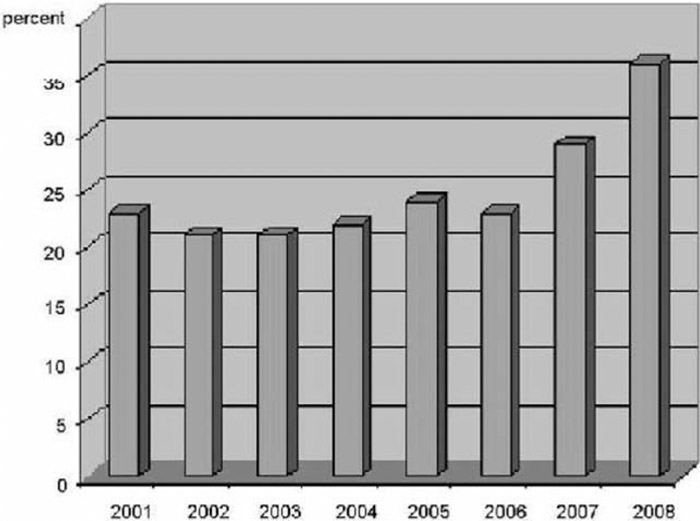
There were 4606 cases of self‐inflicted injury, 1113 of which (25%) were for self‐mutilation. Self‐mutilators were young, male, and more likely to be incarcerated at the time of admission. These patients had psychiatric and substance abuse comorbidities, had multiple admissions, and underwent recurrent foreign‐body removal procedures. The trend of self‐mutilation admissions as a proportion of self‐inflicted injuries over the 7 years of observation increased from 23% in 2001 to 36% in 2008 and was statistically significant (P < 0.0001). There was also an increase seen in self‐mutilation admissions and associated costs relative to all admissions to the hospital (P < 0.0001).
Conclusions:
There appears to be an increase in self‐mutilation encounters over the past few years. Given their central role in caring for hospitalized patients, it is important for hospitalists to be aware of this growing trend. Further investigation into the causes and possible treatments including preemptive educational interventions are also warranted.
Disclosures:
L. Swaminathan ‐ none; A. R. Daniel ‐ none; B. Singal ‐ none