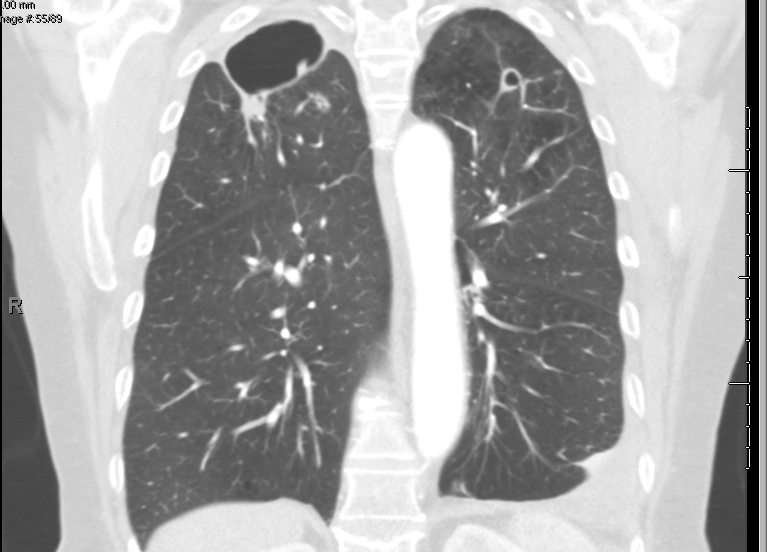
Case Presentation: A 67-year-old female with a 37-year history of seropositive rheumatoid arthritis (RA), managed with tocilizumab for the past two years, presented with a 3-month history of intermittent cough and blood-streaked sputum. Additional symptoms included generalized weakness, shortness of breath, intermittent low-grade fevers, chills, and night sweats. She denied unintentional weight loss, lightheadedness, dizziness, chest pain, or palpitations. She also reported no history of exposure to active tuberculosis, recent travel to tuberculosis-endemic regions, or contact with sick individuals. The patient is an active smoker with a 23-pack-year history.Initial laboratory evaluation revealed no leukocytosis. QuantiFERON-TB testing was negative, as were serologies for hepatitis B, hepatitis C, and HIV. Imaging with contrast-enhanced CT of the chest (Figures 1 and 2) revealed cavitary lesions in both lung apices. The right upper lobe contained a larger lesion measuring 6 × 4 cm, and the left upper lobe showed a smaller lesion measuring 1.5 cm. These findings raised suspicion for either a neoplastic or infectious process.Further evaluation with bronchoscopy showed a normal-appearing bronchial tree without endobronchial lesions. Bronchoalveolar lavage (BAL) from the right upper lobe was performed. Sputum and BAL cultures grew acid-fast bacilli, subsequently identified as Mycobacterium avium complex (MAC) after four weeks, confirming the diagnosis.In response to these findings, tocilizumab was discontinued, and the patient was transitioned to leflunomide and low-dose prednisone for rheumatoid arthritis control. Infectious disease consultation was obtained, and treatment for MAC infection was initiated. The regimen included parenteral amikacin for 12 weeks, combined with oral azithromycin, rifampin, and ethambutol, planned for a duration of at least one year.
Discussion: This case highlights the rare occurrence of pulmonary Mycobacterium avium complex (MAC) infection in a patient with rheumatoid arthritis (RA) on long-term tocilizumab therapy. The immunosuppressive effects of IL-6 inhibition increase susceptibility to opportunistic infections, and this patient’s cavitary apical lung lesions initially mimicked tuberculosis or malignancy. Diagnosis required bronchoscopy and culture studies, confirming MAC as the causative agent. Discontinuation of tocilizumab and initiation of a multi-drug MAC regimen, alongside alternative RA treatment, underscores the importance of balancing immunosuppression with infection risks.
Conclusions: This case underscores the importance of considering opportunistic infections like MAC in immunosuppressed patients on biologic therapies. Early diagnosis, prompt adjustment of immunosuppressive therapy, and appropriate antimicrobial treatment are critical to improving outcomes. A multidisciplinary approach is essential for managing such complex cases.