Background:
Crystalloid fluid solutions are one of the most common medications used in the inpatient setting. Although normally harmless, excessive administration of intravenous fluid (IVF) therapy can be a significant cause of patient morbidity in the hospital. This usually is a result of the liberal use, which based on anecdotal experience, is frequently due to unchecked intravenous fluid orders. The aim of our project was to identify the frequency of timed compared to untimed orders and the associated rates of harm with either fluid order type.
Methods:
The study is a retrospective chart review of all patients at a large urban tertiary referral teaching hospital who were initially admitted to the general medical floor then later transferred to the intensive care unit (ICU) and had previously received intravenous fluid therapy. A pilot data review was conducted for all patients in the month of January 2014. Initial exclusion criteria included age < 18 years, pregnant females, patients on active chemotherapy, and patients with end stage renal disease. Basic demographic information was collected on all patients based on the time of hospital admission. Data regarding duration of intravenous fluids, total amount received, and type of fluid order were manually abstracted from physicians’ orders within the electronic medical record. Patients with fluid orders for less than 8 hours were excluded from further analysis. Adverse events related to fluid overuse, such as need for diuretics at ICU transfer, new hypoxia, and presence of pleural effusions or pulmonary edema on imaging were collected.
Results:
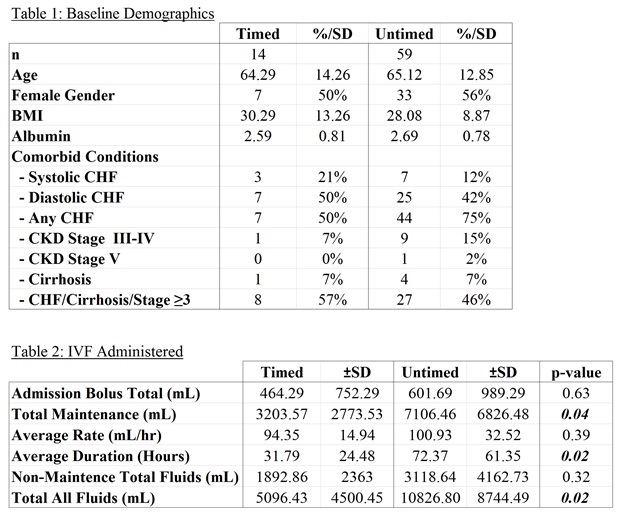
A total of 145 patients were transferred to an intensive care unit during the study period, of those 73 (50%) met the initial inclusion criteria. Of the included patients, 14 (20%) had timed fluid orders, compared to 59 (80%). The groups had similar baseline demographics (Table 1). The timed fluid group received significantly less total IVF doses, maintenance fluids, and duration of IV fluids, but both groups had similar amounts of bolus IVF (Table 2). For the outcomes of diuretic use, hypoxia, pulmonary edema and pleural effusion, there were no statistically significant differences. The composite outcome of hypoxia plus pleural effusion or pulmonary edema had relative risk of 0.39 for timed fluids (p=0.06, 95%CI 0.14-1.04). Of the patients who developed fluid-related complications, 94% had one or more of the following comorbidities (systolic heart failure, diastolic heart failure, cirrhosis, albumin level < 3g/dl, chronic kidney disease stage III or higher).
Conclusions:
There was a trend towards harm in patients who were transferred to the intensive care unit and had received more than 8 hours of untimed fluid therapy on a medical floor. These patients received significantly more fluids over a longer period of time. Patients with hypoalbuminemia, cirrhosis, cardiac, or kidney compromise appear to be more prone to these complications. Although we did not reach statistical significance due to small sample size, using a targeted and restrictive approach to fluid therapy is harmless, if not beneficial.