Background: With COVID surge and staffing shortages, there is a significant strain on hospital systems. Emphasis is on throughput, an effective frontline team, and improved patient and provider communication. Interprofessional rounds are a cornerstone of aligning the care teams and formulating a safe discharge plan.
Purpose: To achieve timely and effective inter-professional communication and close communication gaps between team members, we redesigned rounds by splitting into 2 parts: interdisciplinary disposition and clinical rounds. The goal was to involve key stakeholders (physical therapy), limit the time spent in rounds, while still getting pertinent information, and expediting throughput.
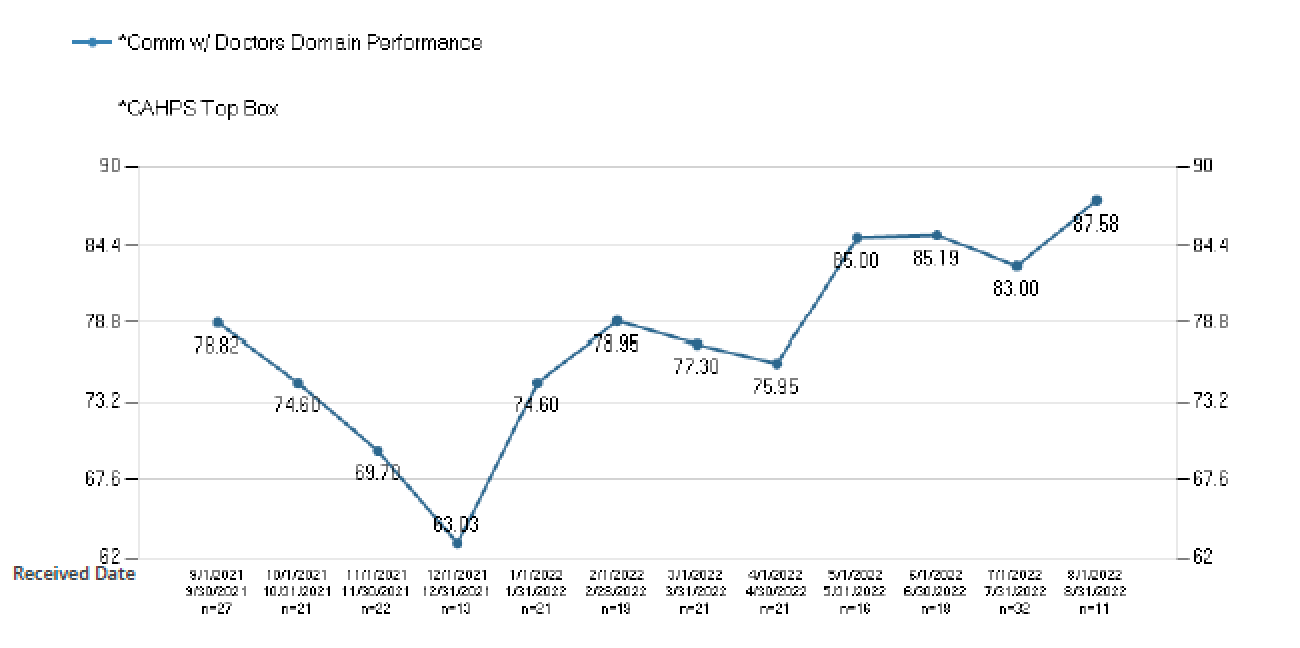
Description: In February 2022, we implemented redesigned split inter-professional rounds using the IHI PDSA Model for Improvement. The first part included interdisciplinary disposition rounds with the physician, nursing coordinator, physical therapist (PT), and case management (CM). The physician focused on the same/next day discharges and identified barriers. Barriers were assigned to specific team members to take ownership (CM ensuring facility arrangements/transportation, PT prioritizing seeing discharge-ready patients first etc).The second part was clinical rounds, which was attended by the physician, primary nurse and pharmacist, and focused on the Safety Board. The Safety Board is an EPIC-generated list that was created by pulling in key patient safety indicator (PSI) data and essential patient information (figure 1). The following outcomes were tracked: median discharge time, percent of patients discharged on the day identified, patient experience, foley catheter and central line use, and incidence of CLABSI and CAUTI. After trending patient experience scores, we added a secondary intervention for physicians of afternoon rounds on discharging patients to help with patient experience.Median discharge time was reduced by 1 hr 10 min, and greater than 80% patients were discharged on the day identified. Central line days in 6 months prior to intervention averaged at 141.8 days, and were reduced to 120.4 days after implementation of Safety Board. No significant reduction in foley catheter usage was noted. One incidence of CAUTI was noted in February (first month of intervention), no incidence of CLABSI was identified. After adding physician afternoon rounds on discharging patients, there was significant improvement in patient experience scores(figure 2).
Conclusions: Implementation of rounds redesign improved the median discharge time and discharge barriers were addressed in a timely fashion. There was downtrend in the number of central line days. With second physician rounds, there was a significant improvement in patient experience. Anecdotally, we saw improvement in team communication and camaraderie, and we plan on measuring this with teamwork surveys in the future.Challenges included some redundancies on the physicians’ end by attending 2 rounds (although the time spent did not significantly increase). Nursing was occasionally missing key information from case management. We had the clinical nursing coordinator discuss with the primary nurse to ensure that the communication loop was closed. In the future, we hope to see improved trends in foley and catheter utilization as well.