Background: Family-centered rounds on our pediatric hospital medicine teaching service, which cares for patients in multiple units throughout the hospital, are often prolonged with unpredictable progression. This contributes to inconsistent nursing participation, inefficiencies in patient care, and variable end times. Through the implementation of scheduled-based rounding, our aims were to: 1) start 90% of rounds encounters within 30 minutes of the scheduled rounding time, 2) increase nursing presence on rounds to >90%, and 3) increase the percentage of rounds completed by 11:20am to 80% by November 2019.
Methods: This initiative started in November 2018 and was focused on the primary pediatric hospital medicine service at a university-affiliated children’s hospital. Our multidisciplinary team, which included attendings, residents, nurses, case management, clinical informatics, interpreter services, and patient and family-centered care representatives, focused on the following key drivers: a shared mental model surrounding team member roles and daily rounding plan, senior resident ownership of the schedule, and enhanced family education. Interventions included: 1) customization and regular improvements of a semi-automated scheduling tool within the electronic medical record; 2) daily schedule management by the senior resident and resident data transparency; 3) real-time rounds notification to nurses via secure text messaging systems; 4) routine e-mail reminders to senior residents upon start of service weeks; 5) interpreter workflow modification to support scheduled rounding times; 6) weekly in-person meetings with the service team and key stakeholders to identify issues in real-time; and 7) family notification of rounding time and enhanced family education on the rounding process. Data were collected daily during rounds by a case manager or an attending physician.
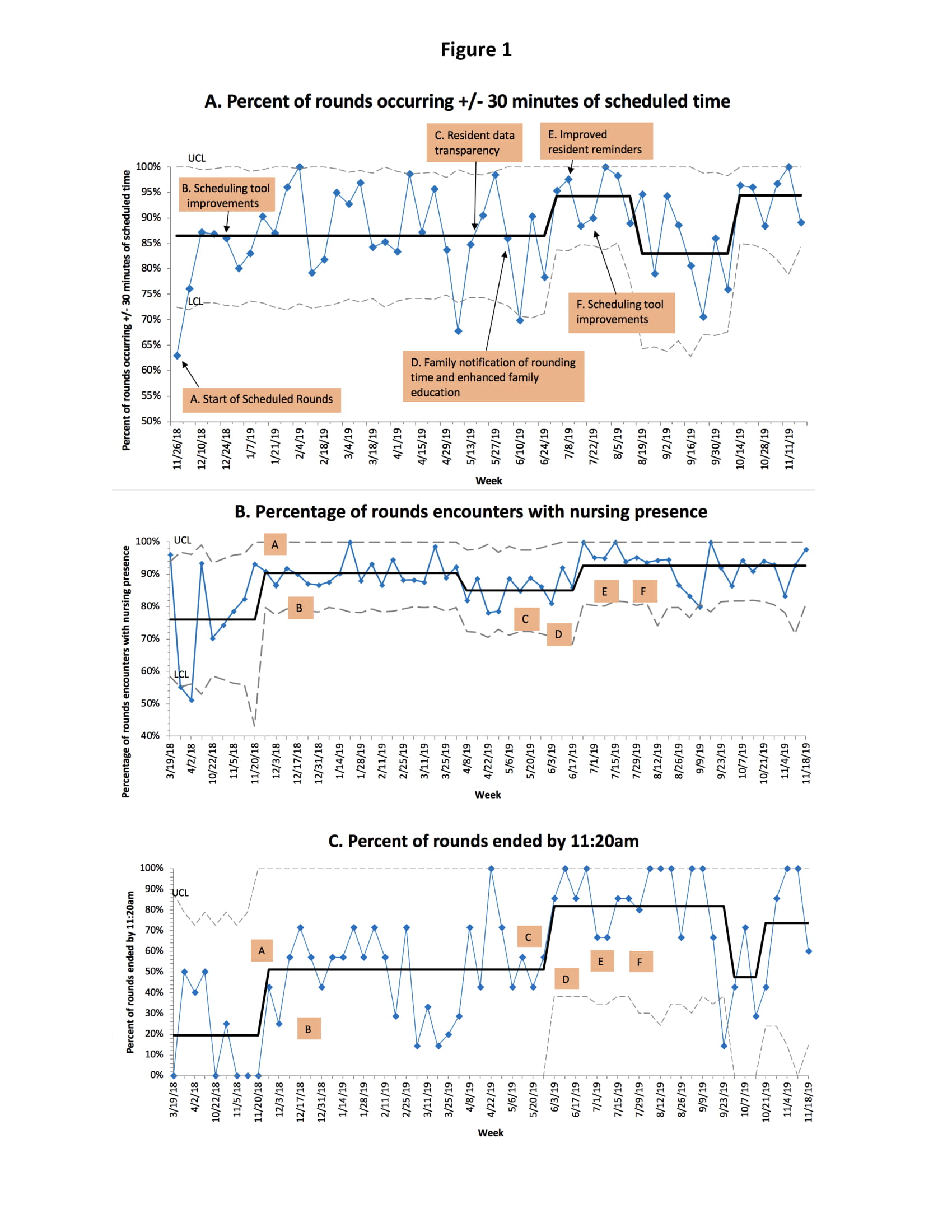
Results: As of November 2019, 94% of rounds occurred within 30 minutes of scheduled rounding time, nursing presence increased from 76% to 93% and the percentage of rounds completed by 11:20 am increased from 19% to 74% (Figure 1). After the implementation of scheduled rounds, the percent of residents who were “somewhat” or “extremely satisfied” with rounds increased from 25% to 75% (p<0.001). Weekly meetings revealed the following challenges: frequently rotating trainees, resident unfamiliarity with the process, maintaining end times during high census, patients in multiple units, and extended discussions on complex patients.
Conclusions: A multi-faceted scheduled-based rounding intervention which focuses on shared expectations, enhanced communication between team members, resident ownership and family education can improve efficiency and nursing presence during family-centered rounds.