Background: Screening and treatment for unhealthy alcohol use (UAU) and alcohol use disorder (AUD) is recommended but underutilized, particularly in inpatient settings. Initiating interventions during hospitalization can reduce UAU and may improve clinical outcomes.
Methods: We implemented screening and treatment for UAU at a safety-net hospital in Austin, Texas. Nurses screen admitted patients with the AUDIT-PC. Substance use navigators (SUNs) who are social workers evaluate patients with a positive score (≥5) or who are admitted for alcohol-related reasons. The evaluation includes a full AUDIT and a brief behavioral intervention. Patients with an AUDIT ≥12 are offered medications for AUD (MAUD) at discharge. The SUNs also provide recovery resources and facilitate primary care follow-up.For patients with an AUDIT ≥12, we sought to contact and administer a repeat AUDIT at 4-6 weeks post-discharge. We also conducted chart reviews to assess 30-day readmissions, follow-up rates, and medication adherence.
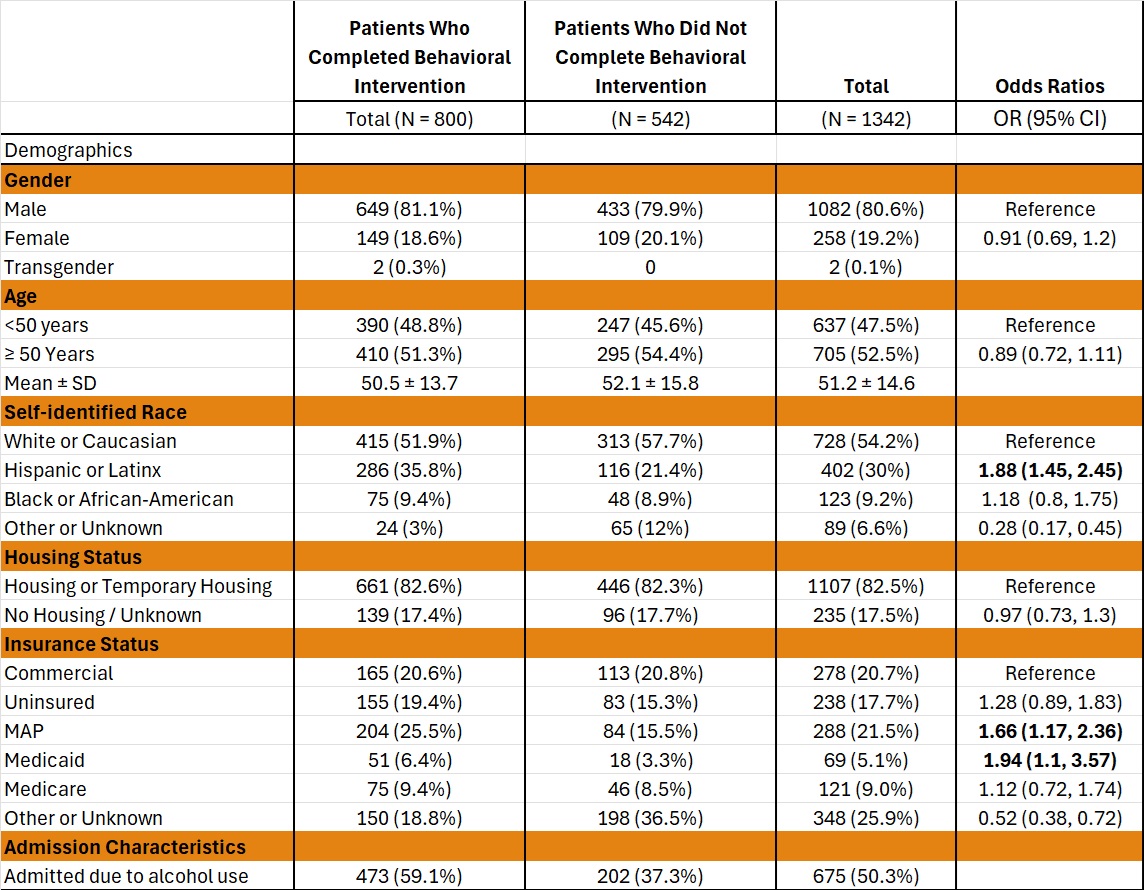
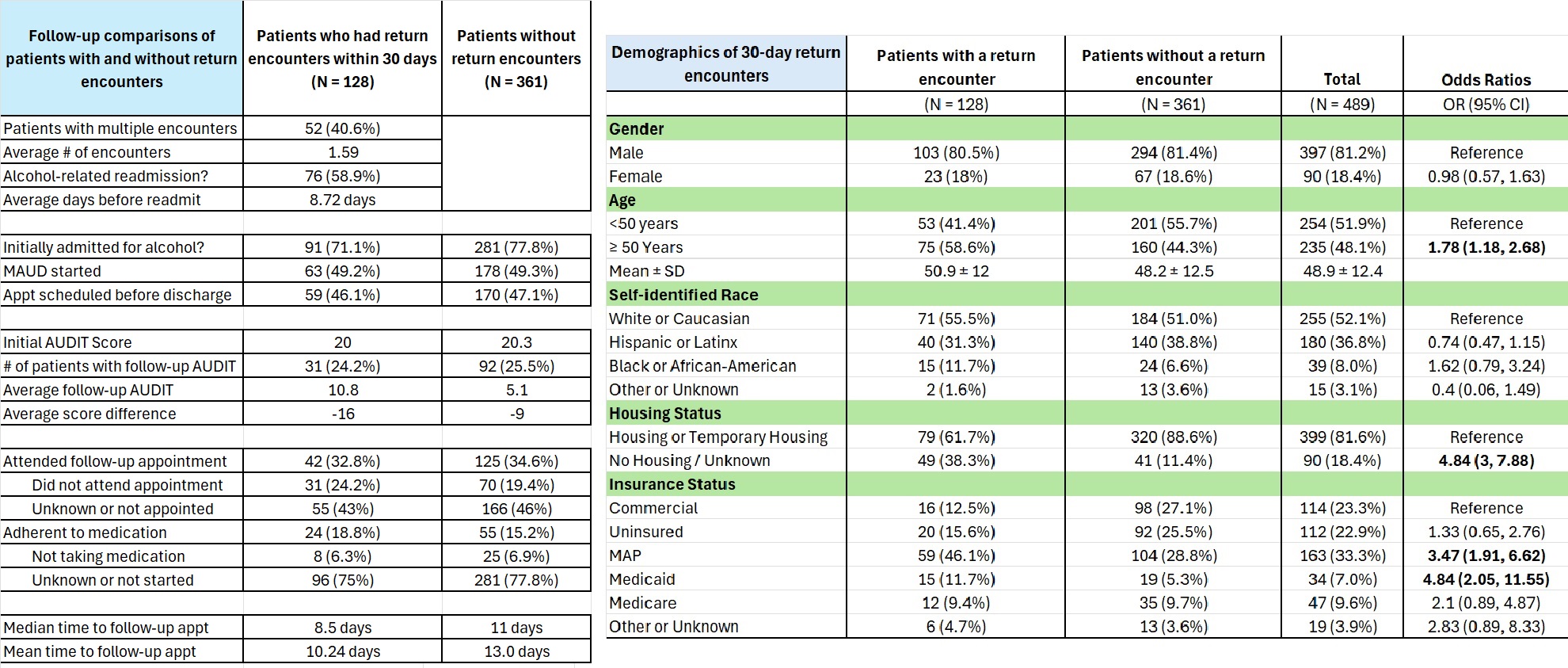
Results: From 9/2022 to 9/2024, 27,914 patients were admitted. 18,146 (65%) were screened with the AUDIT-PC, with 1085 (6.0%) screening positive. SUNs identified 257 additional patients with UAU through referral methods.Of these 1342 patients, 81% were men, and mean age was 51 years. 54% were Caucasian, 30% were Hispanic / Latinx, and 9% were Black. 17% were unhoused, 18% were uninsured, and 21.5% were covered by a county-based medical assistance program (MAP).Of these 1342, 800 (59.6%) patients engaged in and received the intervention. The mean AUDIT score was 15, and 473 / 800 patients (59%) were admitted to the hospital due to consequences of alcohol use. Those who engaged in the intervention were more likely to be Hispanic / Latinx (OR: 1.88, 95% CI: 1.45-2.45), and have MAP or Medicaid (OR: 1.66, 95% CI 1.17-2.36; OR: 1.94, 95% CI 1.1-3.57).In addition, for the 489 (61%) patients with AUDIT ≥12, 273 (56%) were eligible and interested in MAUD, and 248 were started on medication before discharge. The SUNs placed primary care referrals for 315 (64%) patients. We completed follow-up phone calls for 149 (30%) patients with AUDIT≥12, and 124 (83.2%) completed a repeat AUDIT. Mean reduction in AUDIT was 13.8 points (95% CI: -15.4, -12.2). 36 patients had stopped drinking entirely. Outpatient chart reviews were completed for an additional 164 patients (33.5%). Of the 313 patients with follow-up data, 163 (52.1%) attended their follow-up appointment, and 76 (24.3%) reported adherence to MAUD.For the 489 patients with AUDIT≥12, inpatient chart review showed 128 (26%) patients had a return hospital encounter (emergency room visit or readmission) within 30 days of discharge. Nearly 60% of these encounters were due to continued alcohol use. Patients with a return hospital encounter were more likely to be >50 years of age (OR: 1.78, 95% CI:1.18–2.68), unhoused (OR: 4.84, 95% CI: 3-7.88), and have Medicaid or MAP (OR: 4.48, 95% CI: 2.05-11.55; OR: 3.47, 95% CI: 1.91-6.62). Patients with a return encounter also had smaller reductions in AUDIT score than those who did not have return encounters, with mean reduction of -9.0 vs -16.1 points (difference 7.0, 95% CI: 3.1-11.0). There were no major differences in initial AUDIT score or MAUD initiation between patients with and without a return encounter.
Conclusions: Screening and treatment for UAU can be effectively delivered in a hospital setting and can reduce alcohol use in the short term. More work is needed to improve adherence with medication and follow-up in these high-risk patients.