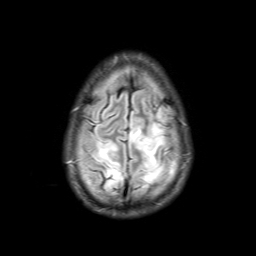
Case Presentation: A 50 year-old man with a history of kidney-pancreas transplant was transferred to our hospital for acute onset right side numbness, twitching and altered mental status. Prior to his presentation, he was hospitalized for a perforated appendicitis with abscess and was discharged one day before on IV ertapenem and oral linezolid. The patient was intubated for airway protection due to worsening mental status. An LP was notable for an elevated protein and cultures were negative. A head CT scan was negative and EEG did not show epileptiform seizure activity. He had two generalized tonic-clonic seizures en route of transfer and was treated with IV lorazepam. Upon arrival, the patient was febrile to 39.5 C and hypertensive with systolic blood pressures of 160s-170s. His WBC count was 31.2. An extensive workup including blood and urine cultures, chest x-ray, CT abdomen/pelvis, transplant kidney US, and echocardiogram showed no evidence of active infection. Ertapenem was switched to piperacillin/tazobactam and linezolid was continued. A repeat EEG showed severe encephalopathy but no focal features or epileptiform discharges. A brain MRI showed bilateral subcortical white matter changes in the posterior cerebral hemispheres with adjacent gyriform infarction (see figure). Given the MRI findings, tacrolimus use and recent hypertension, posterior reversible encephalopathy syndrome (PRES) was diagnosed. The patient was treated with nifedipine and tacrolimus was changed to everolimus. The patient had a full neurologic recovery after 2 months.
Discussion: PRES is a rare condition characterized by reversible white matter lesions on brain MRI associated with headaches, altered mental status, visual disturbances and seizures. Neuroimaging with MRI typically shows symmetric bilateral subcortical/cortical hyperintensity in T2-weighted images, more often in parieto-occipital lobes. Risk factors include preeclampsia-eclampsia, renal failure, ischemic bowel disease, sepsis, uremia, and hyponatremia. Multiple drugs are also associated with PRES including immunosuppressants (cyclosporine, tacrolimus, IVIG and interferon alpha) and cytotoxic drugs (cisplatin, cytarabine and methotrexate). Our patient was taking tacrolimus and his BP was uncontrolled. He was also prescribed ertapenem which has been shown to elevate tacrolimus levels by inhibition of its metabolism. The treatment of PRES includes blood pressure control and treatment of any underlying associated conditions.
Conclusions: The purpose of reporting this case is to promote awareness of PRES. Early diagnosis and appropriate treatment will usually result in a favorable prognosis although PRES is not always reversible. In this case, the drug interaction between tacrolimus and ertapenem was likely a major contributing factor in the development of PRES.