Background:
Sepsis is a systemic host response to infection that may result in significant morbidity with mortality rates from severe sepsis or septic shock reaching over 20% in most studies. Research on sepsis has focused on use of groups of sepsis specific interventions (termed care bundles) that are given in response to the declaration of sepsis. Early intervention in sepsis has been shown to improve patient outcomes, and sepsis bundles have been widely adopted in many hospitals to help facilitate early recognition and intervention in sepsis. In addition, recent research has explored the difference in patient care between the day and on nights or weekends. Research on this topic has been mixed, but some studies have shown significantly worse outcomes for patients during nights and weekends.
Methods:
Our study looks at the relationship between the time sepsis is declared and their subsequent bundle compliance and survival to discharge. We hypothesize that there will be a decrease in sepsis bundle compliance between in-patients declared to have severe sepsis or septic shock on nights and weekends and that this will lead to a difference in the rate of survival to discharge. This study was performed at LAC+USC Medical Center utilizing data collected for reporting purposes. All patients declared to have severe sepsis or septic shock during their inpatient stay in the hospital from December 2011 until the end of December 2013 were included in our study.
Results:
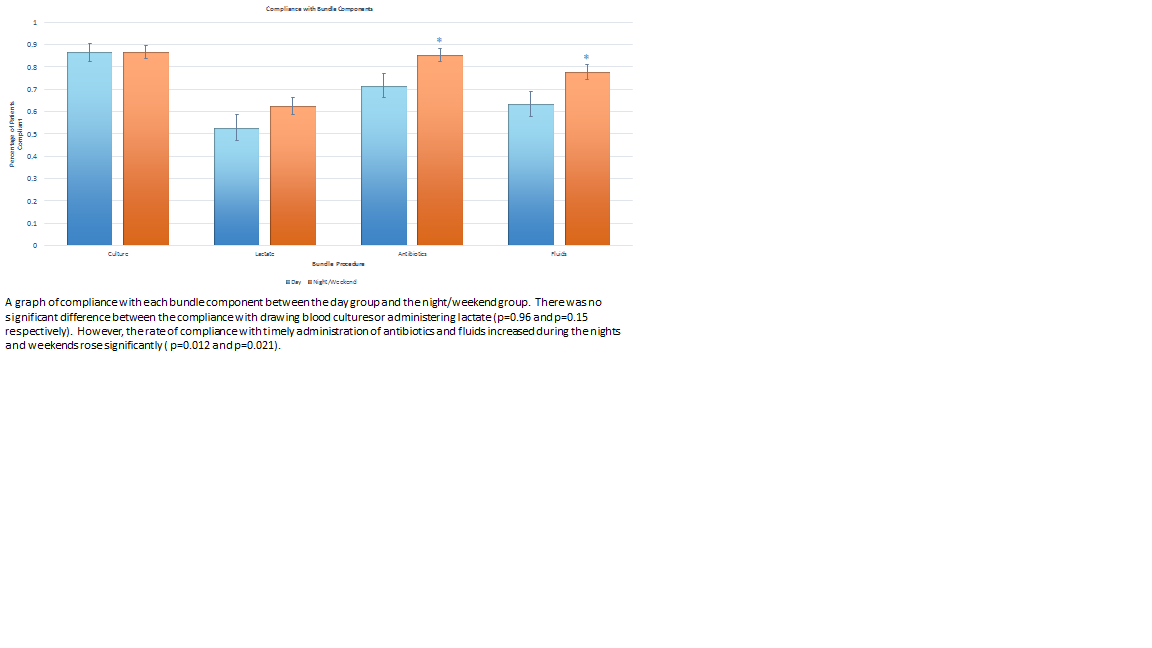
We found a significant decrease in the overall bundle compliance during the day when compared with nights and weekends (18.9% vs 38.0% P=0.0037). In particular we found a decrease in the timely administration of appropriate antibiotics (71.6% vs 85.4 p=0.012) and fluid resuscitation (63.5% vs 77.8% p=0.021) in those patients diagnosed during the day. The in-patient survival to discharge did not differ significantly between the two groups (63.5% vs 62.0% P=0.827).
Conclusions:
Contrary to our hypothesis, compliance with the sepsis bundles increased for patients during nights and on weekends. There are many possible reasons why there may be an increase in sepsis bundle compliance on nights and weekends. One possibility is that there are less educational responsibilities such as teaching rounds or conferences that could potentially delay action on potentially septic patients. This minimization of distraction may allow physicians to focus on meeting the parameters necessary for bundle compliance. Also of note, this increase in compliance did not lead to an improvement in the rate of survival to discharge, which is consistent with recent research on the lack of mortality benefit in bundle compliance.