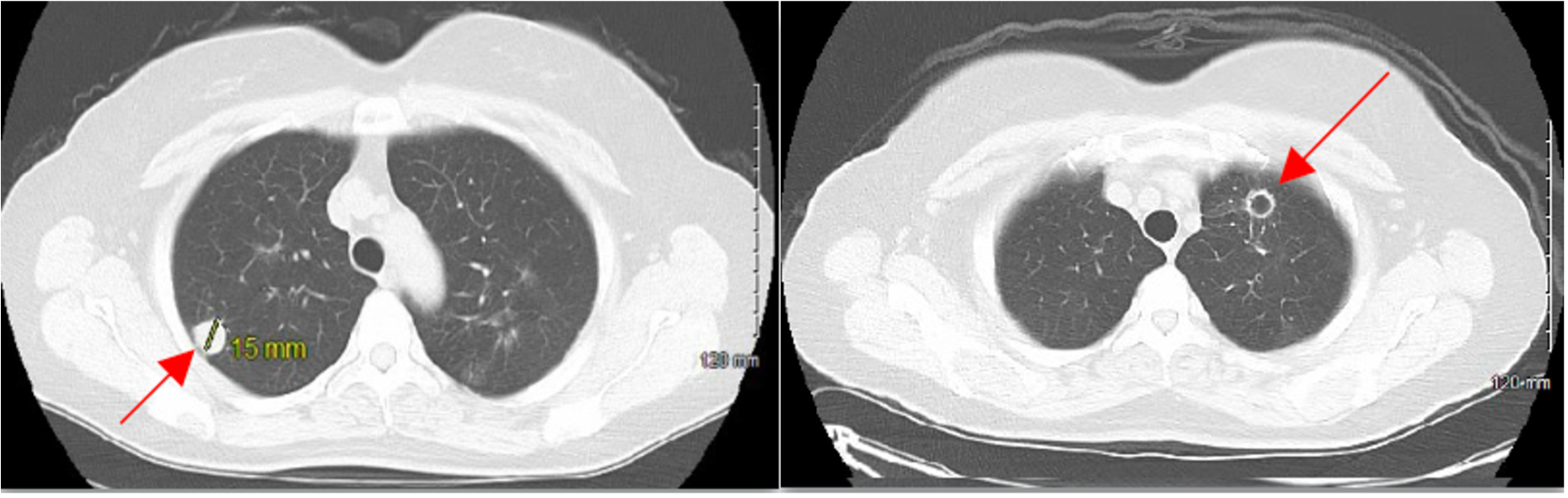
Case Presentation: 54-year-old female with past medical history of bronchitis was referred for evaluation of hemoptysis and chest radiograph changes. She had 5 pack year history of cigarette smoking but quit 4 years prior. Additionally, she admitted to significant occupational exposure working as an electrician for 8 years. On physical examination, her temperature was 37.3°C, blood pressure was 126/77 mmHg, heart rate was 85 beats per minute, and oxygen saturation was 94% on room air. Her lab values were significant for a positive QuantiFERON test; negative antineutrophil cytoplasmic antibodies (ANCA) and antinuclear antibodies (ANA) tests.Computed Tomography (CT) scan of chest revealed multiple bilateral pulmonary nodules with some cavitation. The largest solid nodules measured 13 mm and 15 mm in the left and right upper lung, respectively. A CT-guided biopsy was performed on a right lower lobe nodule which revealed non-neoplastic chronic inflammation with an area of geographic necrosis. An additional robotic-assisted left upper and lower lobe wedge resection was performed revealing white to tan granular lesions with necrotizing granulomatous inflammation and lymph nodes with anthracosis and abundant histiocytes consistent with GPA.Following rheumatology consultation, the patient was treated with intravenous rituximab once weekly for 1 month, followed by once a month for 6 months. A repeat CT scan done 4 weeks following treatment showed no development of new lesions and size reduction or resolution of previously noted nodules.
Discussion: While ANCA serology is the widely accepted diagnostic criteria, this case highlights the importance of a high index of suspicion without the presence of ANCA as an indicative marker. According to the criteria established by American College of Rheumatology, diagnosis of GPA presence of two or more of these four criteria was associated with an 88% sensitivity and 92% specificity: (i) a urinary sediment containing red blood cell casts or more than five red blood cells per high-power field, (ii) abnormal findings on the chest radiograph, (iii) oral ulcers or nasal discharge and (iv) granulomatous inflammation on biopsy. As our patient satisfies two of the above 4 criteria and with biopsy showing necrotizing granulomatous inflammation, a diagnosis of seronegative limited granulomatosis with polyangiitis without renal involvement was made.
Conclusions: GPA is associated with a mortality rate of 80% in untreated patients, therefore early diagnosis and treatment are critical. The limited form of GPA has excellent prognosis if diagnosed early and treatment is started. However, GPA with renal and multi organ involvement has poor prognosis and a high mortality rate. In this case, our patient presented with isolated lung lesions leading to a better prognosis and response to treatment. Though ANCA is a highly predictive marker for GPA, in patients presenting with cavitary lung lesions which are ANCA negative, GPA should still be suspected to improve patient outcomes.