Case Presentation: A 69-year-old woman with metastatic breast cancer, atrial fibrillation (on coumadin) and CKD stage III was admitted after a fall. She was treated for pneumonia with ceftriaxone and azithromycin. On hospital day 2, the patient became encephalopathic, hypotensive and required endotracheal intubation for hypercapneic respiratory failure. Antibiotics were broadened to vancomycin and piperacillin/tazobactam.On hospital day 3, the platelet count abruptly dropped from 168×103/μL to 1×103/μL with initially stable hemoglobin and WBC count. Labs and peripheral smear did not suggest a microangiopathic hemolytic process or worsening coagulopathy. The patient developed small-volume hemoptysis and extensive ecchymoses. Drug-induced thrombocytopenia was suspected and vancomycin was discontinued. Notably, the patient was not exposed to any heparin products as her INR was therapeutic. She received prothrombin complex concentrate and plasma to reverse her coagulopathy, along with a total of 8 units of platelets and 2 units of pRBCs. Intravenous immunoglobulin was given but the platelet count never recovered. The patient developed worsening hypoxic respiratory failure and died in hospice on hospital day 7. Labs subsequently confirmed the presence of vancomycin-dependent anti-platelet IgM and IgG antibodies.
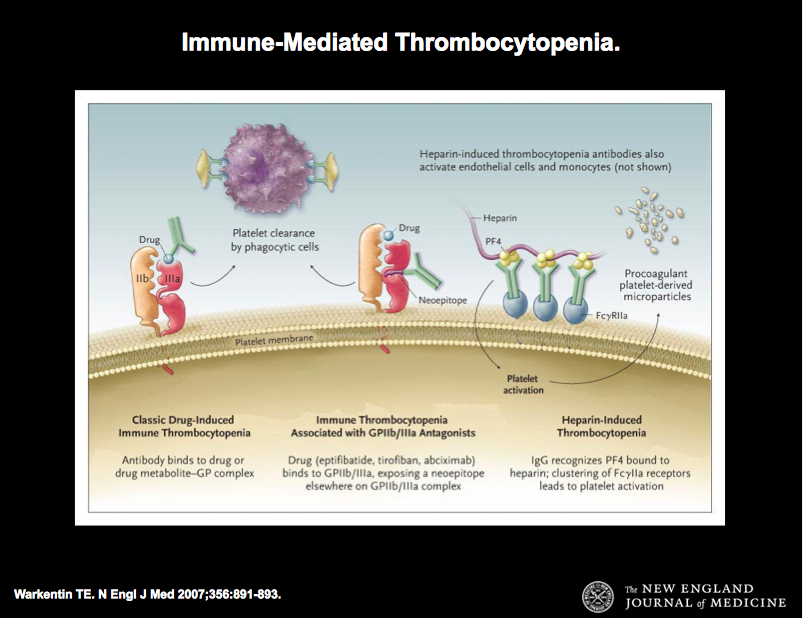
Discussion: Thrombocytopenia induced by vancomycin exposure is thought to be due to the synthesis of IgG and IgM antibodies that interact with the glycoprotein IIb/IIIa receptor on the platelet surface in a vancomycin dependent manner, with subsequent platelet activation and destruction. Thrombocytopenia typically occurs after several days of exposure to vancomycin but platelet counts can drop precipitously in patients who have been previously exposed. We suspect this patient had prior vancomycin exposure given the rapid drop in platelet count. The degree of thrombocytopenia induced by vancomycin can be very severe and platelet transfusion is often ineffective. Cessation of vancomycin is essential, which results in normalization of the platelet count in most patients. Intravenous immunoglobulin and plasmapheresis have been used to neutralize or remove the vancomycin-dependent antibodies. Delayed clearance of vancomycin from renal failure can delay the recovery of platelet counts, which was likely a factor for our patient.
Conclusions: Our case highlights drug-induced thrombocytopenia as a rare but life-threatening complication of vancomycin administration. Immediate discontinuation of vancomycin is paramount; however, platelet destruction may be so rapid and refractory to treatment that clinical consequences can be dire.