Background: Since the ACGME established duty hour limits in 2003, there has been an increasing prevalence of night float rotations in internal medicine residency training. Conferences and formal didactics are a critical component of resident education. However, residents on night float rotations typically miss these essential educational activities that are typically held during the daytime [1]. It is thus unsurprising that survey data has shown that both residents and faculty rate teaching and learning on day rotations more positively than night rotations [2,3,4,5,6] citing concerns of less educational emphasis, lack of conferences, and decreased availability of attending physicians [7]. Many programs have responded by initiating night curricula, but there remains a paucity of data on how to best implement formal resident education overnight.
Methods: We introduced a novel night float educational initiative at a single academic medical center, wherein attending nocturnists lead 60-90-minute sessions with night float internal medicine residents five to seven nights per week. Sessions consist of brief resident presentations of overnight admissions with discussion of their assessment and plans after which attendings provide feedback and offer alternate differentials or treatments. The sessions also provide a forum for questions regarding the care of cross-coverage patients and an outlet for the nocturnists to provide additional educational pearls. We assessed resident satisfaction via an anonymous nine-question survey as well as reviewed the standard GME survey distributed to housestaff yearly over the implementation period.
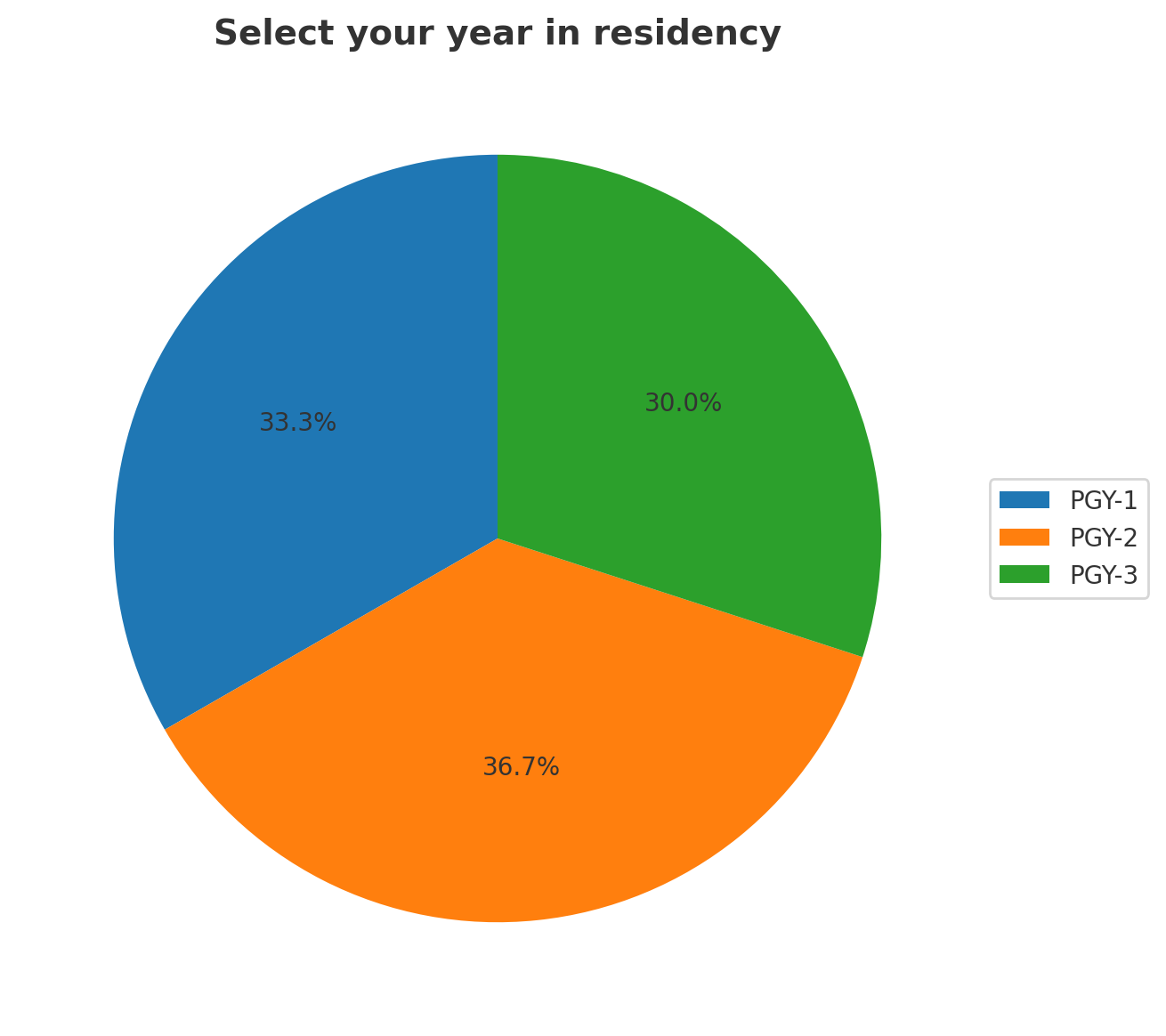
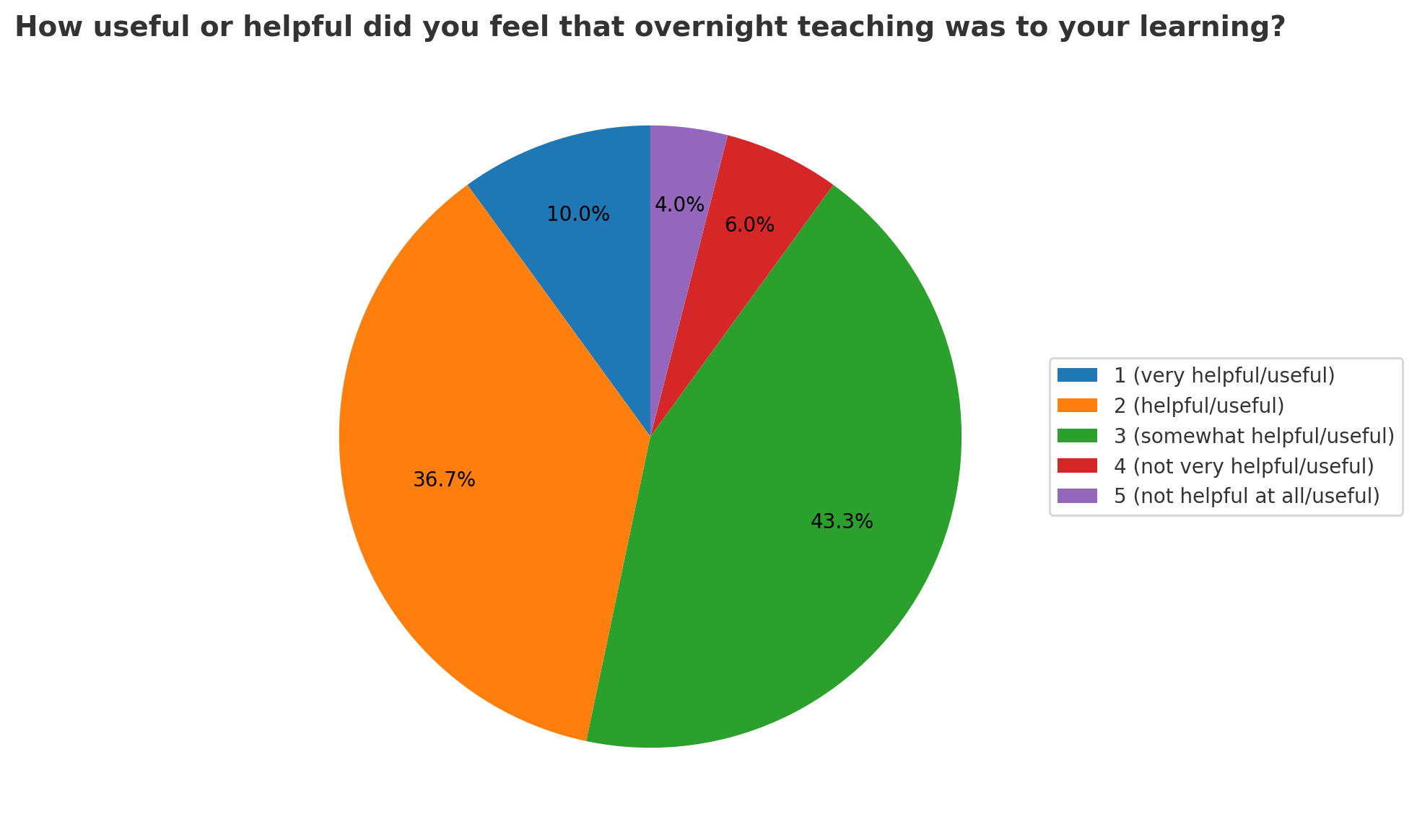
Results: Thirty responses were received from 105 residents who had had at least one night float rotation, ranging from PGY1 to PGY3. Of residents surveyed, 100% felt more comfortable knowing there was an internist available overnight. Sixty-five percent preferred a flexible schedule for the teaching sessions to a fixed schedule. Of surveyed residents, 43% described the sessions as “somewhat useful”, 37% described them as “useful” and 10% described them as “very useful.” Additionally, anonymous GME surveys results showed an improvement from 65th percentile to above 90th percentile for the question related to “supervision at night” post implementation of night teaching program.
Conclusions: Our findings are supportive of previous data suggesting that modifications to night float curriculums can improve the educational value of the rotation. Most of the residents answered favorably when asked how they viewed the teaching sessions. Limitations of our study include the response rate of 29% and lack of a randomized control group. We also surveyed a single residency program with a small group of nocturnists potentially limiting the generalizability of our findings. However, trends in responses may be helpful for implementing and guiding future night training programs.