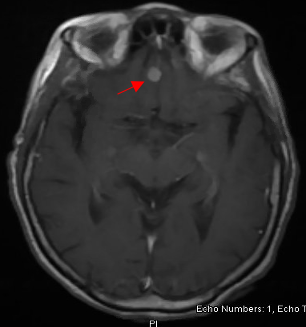
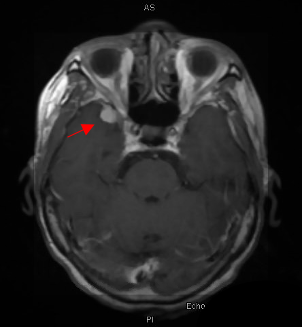
Case Presentation: A 78-year-old African American female with a history of hypertension, coronary artery disease, heart failure with reduced ejection fraction, chronic kidney disease (CKD) stage 4, and systemic sarcoidosis in remission, presented for an acute change in mental status with delusions, and memory loss for 1 week. She had a history of dysphagia with loss of appetite and weight (30 lbs) in the last 9 months. She was diagnosed with sarcoidosis 10 years ago, following the development of skin and ocular lesions, progressive weakness and deformity of the left hand, with right-sided mediastinal nodularity on chest x-ray and meningeal based sarcoid on magnetic resonance imaging (MRI) of the brain. She was then successfully treated with steroids without any complications.On exam, she was alert and oriented to person and place, delusional, minimally cooperative with blunt affect and sluggish speech, and without any evidence of focal neurological deficits (FND). Labs were remarkable for chronic leucopenia and thrombocytopenia, acute kidney injury (AKI) on CKD, and mildly elevated liver enzymes, erythrocyte sedimentation rate, ammonia and ACE levels; otherwise, thyroid profile, vitamin B12, folic acid, ANA and anti-smooth muscle antibody (ASMA) titers, serum and urine electrophoresis, HIV, viral hepatitis panel, urinalysis, and urine toxicology were normal. Her computed tomography (CT) scan of the head did not show any acute changes. The gastrointestinal evaluation of weight loss, performed with a modified barium swallow, esophagogram and CT Abdomen and Pelvis, was unremarkable. CT Chest redemonstrated the left lower lobe opacity without any new changes. MRI Brain with gadolinium contrast revealed multiple leptomeningeal enhancements with a new extra-axial lesion near the right temporal lobe. She was diagnosed with recurrent neurosarcoidosis (NS) and started on the steroid pulse regimen. Her mental status initially improved but declined later with steroid tapering. She was discharged to a hospice where she died 2 months later.
Discussion: NS is relatively unusual, with devastating manifestations and a diagnosis of exclusion [1]. With a prevalence of ~2 per 100,000 population, predominantly in African Americans and females, it may present with FND, peripheral neuropathy, meningitis, neuroendocrine disorders, myelopathy, myopathy, seizures, hydrocephalus and rarely, cognitive decline and coma [5]. Gadolinium contrast MRI is the most sensitive but nonspecific test; brain biopsy remains the gold standard [2,4]. Steroid remains the mainstay of treatment, followed by immunosuppressants, radiotherapy and surgery. Monitoring is needed to ensure the resolution of markers of disease activity. It can be chronic or fatal, more likely in African Americans (~5% of patients) [6]. Remissions and recurrences are quite uncommon (<5% of patients), but it may happen at any age.
Conclusions: Diagnosis of NS remains challenging even in patients with a history of sarcoidosis due to rare occurrences with diverse clinical presentations, lack of specific laboratory or radiologic findings and complications associated with invasive brain biopsy. Recognition and treatment are imperative to avoid further neurological damage. Management is critical due to poor prognosis with a high mortality rate. Long-term follow-up is recommended in patients with inactive disease to identify remissions or recurrences.