Background: The accelerating integration of point of care ultrasound (POCUS) training into UME and GME curricula puts academic faculty untrained in POCUS at a disadvantage. Educating providers in POCUS during the clinical day is challenging. A faculty development program that creates a safe learning space for providers with variable schedules and unpredictable clinical responsibilities would provide a much needed service to academic hospitalists.
Purpose: The design of the Faculty Development POCUS Workshop Series had the following aims: 1) Design each session to stand alone, 2) Create an educational model emphasizing hands-on experiential learning, 3) Make time management a shared priority, 4) Create space for faculty to experience uncertainty while gaining exposure to POCUS.
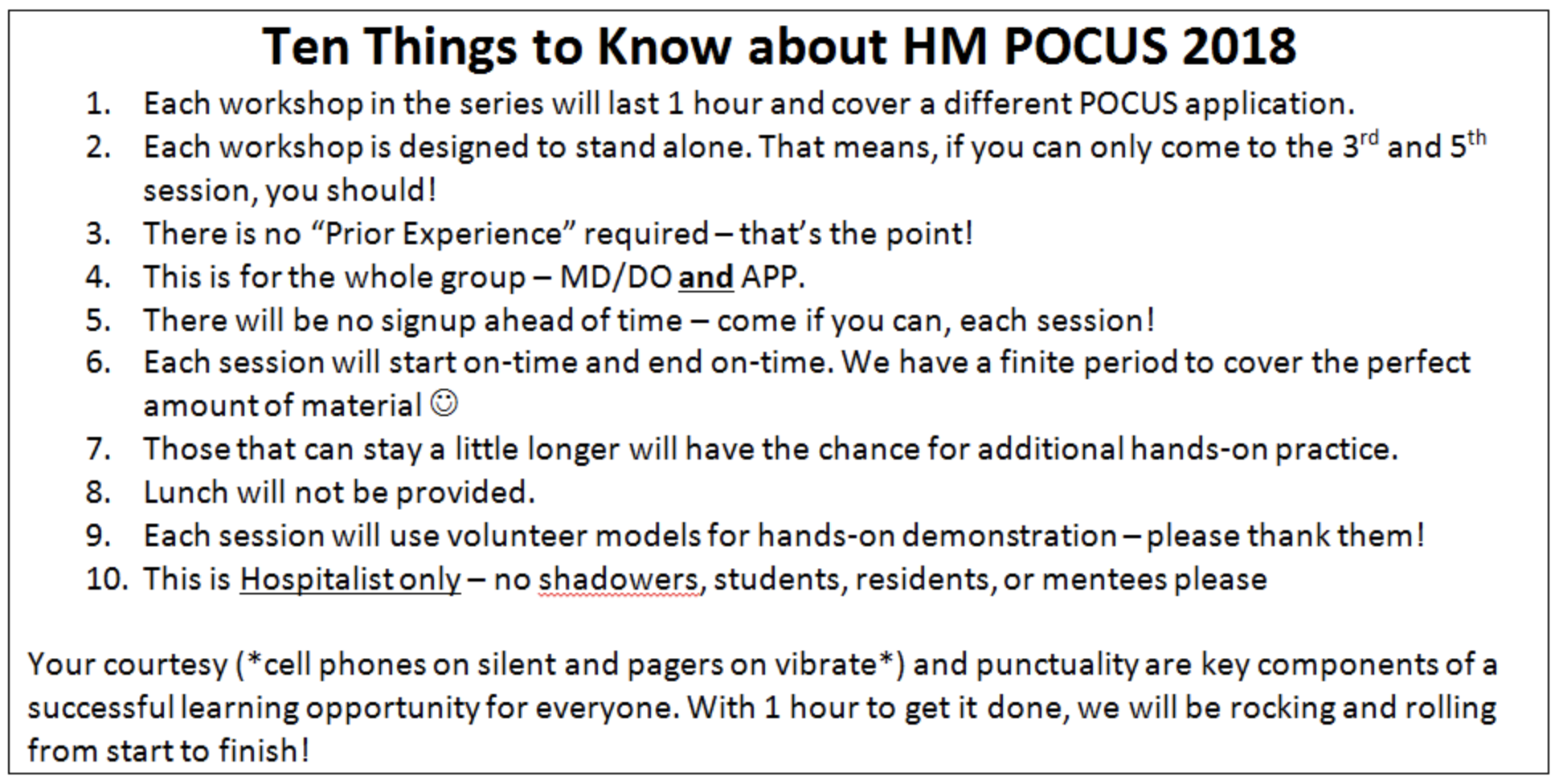
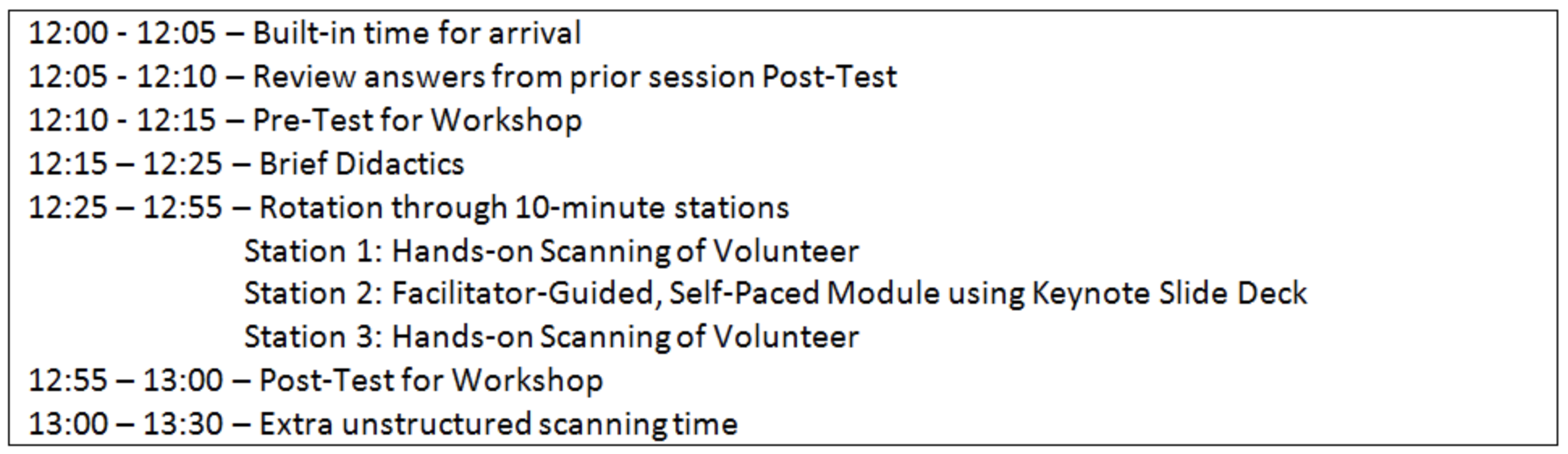
Description: Denver Health is a 527 bed academic safety net hospital. Our group is 45 physicians and 11 APPs. Our workshop series occurred biweekly for a total of 6 sessions over 12 weeks. Calendar invites included shared expectations of the workshop facilitators and participants (see Table 1). Each workshop followed the same 55-minute program (see Table 2). The first 20 minutes allowed participants to eat lunch during the pre-test and didactics, followed by 30 minutes of stations. One facilitator managed time by announcing each transition. There were 3, 10-minute, interactive stations: 2 with instructors guiding attendees scanning on live volunteers and 1 station that consisted of a slide deck module. Additional unstructured hands-on time was available for 30 minutes after each session.
Each workshop focused on one POCUS application. No workshop required attendance at a prior one. We did not separate people by experience level allowing for skill-mixing within each station. We intentionally excluded non-faculty learners from workshops to protect space for faculty to be challenged and potentially ‘fail’ with real-time guidance. A final anonymous course evaluation allowed faculty participating in any session to provide feedback on all aspects of the workshops.
Conclusions: The course was well received. The average attendance was 17. While this represents 31% of the total group, there are typically 16 hospitalists on a day shift at one time. On the evaluation, queries entitled “The design of the workshops is innovative” and “The design of these workshops respects my time as a busy clinician” both received 20 of 20 “Agree” or “Strongly Agree” responses. Free-form responses were also universally favorable. Those that attended zero sessions and filled out the course evaluation all reported having schedule conflicts which represents a potential area for persistent innovation.
POCUS education for attending providers is being outpaced by education being provided to learners, creating a deficit in the ability of faculty to employ POCUS as an educational tool. This reproducible workshop design offers a way to improve POCUS education for hospitalists.