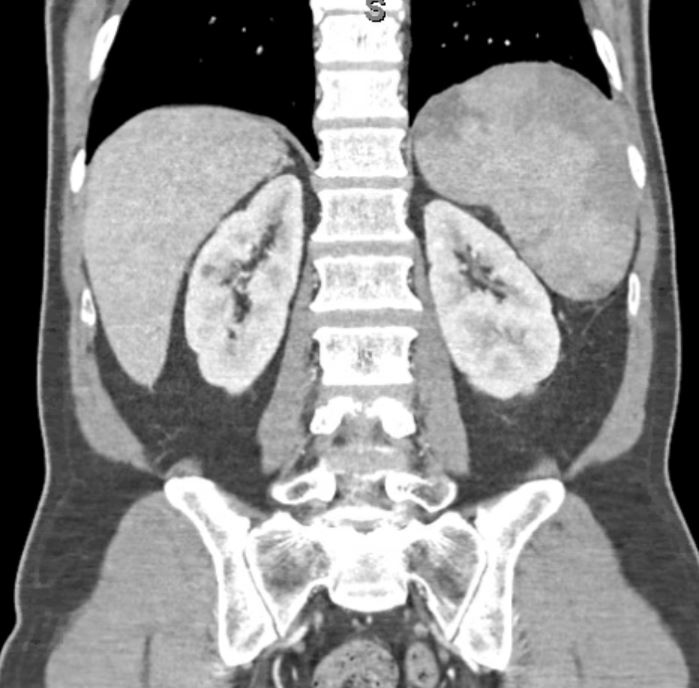
Case Presentation: The patient is a 65-year-old Vietnamese male presenting with fever, chills, night sweats and fatigue for one week. He also reports a dry cough with dark urine but denies recent weight loss, abdominal pain, nausea, vomiting and diarrhea. He denies recent travel history and has had no sick contacts. Patient last visited Vietnam two years prior but did not visit any rural regions. He is an avid gardener but does not recall any recent tick bites. Labs showed anemia, thrombocytopenia and elevated aspartate aminotransferase (AST), alkaline phosphatase, lactate dehydrogenase (LDH) and total bilirubin. CT abdomen and pelvis revealed enlargement and heterogenous appearance to spleen with wedge shaped infarcts and distended gallbladder with minimal common bile duct enlargement. Magnetic resonance cholangiopancreatography (MRCP) showed no evidence of choledocholithiasis. Blood smear returned positive for possible babesia versus plasmodium and parasitemia of 0.8%. Patient was treated with atovaquone-proguanil, doxycycline and azithromycin to cover for possible tick born coinfections and showed improvement over the next few days. Final smear results were positive for Babesia and the remaining tick born infection workup was negative.
Discussion: Splenic rupture is a rare complication of babesiosis that is often seen in otherwise healthy individuals. The splenic infarcts seen on this patient’s CT scan can be thought of as a precursor that could have potentially led to splenic rupture. Patients who develop splenic rupture often present with mild splenomegaly, have low parasitemia and do not present with the other manifestations of severe babesiosis which can cause a delay in diagnosis and treatment.
Conclusions: Splenic rupture can rapidly progress to hemorrhagic shock and death. Thus it is important to include work up for tick borne infections in a patient presenting with febrile viral-like illness accompanied by nonspecific symptoms.